Why combo pills cost way more than you think
Imagine you need two medicines: one for blood pressure, another for cholesterol. Your doctor gives you a single pill that combines both. It’s convenient. But that convenience comes at a price-often 10 to 15 times more than buying the same two drugs separately as generics.
In 2016, Medicare paid $925 million more for brand-name combination pills than it would have if patients had taken the same ingredients as individual generic pills. That’s not a typo. That’s $925 million wasted on pricing that doesn’t reflect actual cost. And it’s happening right now, in 2026, across the U.S. and other countries with similar drug pricing systems.
How combo pills trick the system
Fixed-dose combinations (FDCs) sound like smart medicine: fewer pills, better adherence. But here’s the catch-many of these combos pair a brand-new, expensive drug with an old, cheap generic. Take Janumet: it combines sitagliptin (brand-new in 2007) with metformin (generic since the 1970s). Metformin costs $4 for a 30-day supply at Walmart. Janumet? Around $472 for the same length. That’s a 11,700% markup on one ingredient.
This isn’t accidental. Drug companies use a strategy called “evergreening.” When a drug’s patent expires, they slap it into a combo with a newer, still-patented drug. Suddenly, the whole package stays protected. Even if one component is generic, the combo gets to keep its high price. The FDA doesn’t stop this. Insurance plans often don’t question it. And patients? They assume the combo is just better.
The math doesn’t add up
Here’s how pricing works in the real world:
- Two separate brand-name pills? $100 total.
- Same two drugs in one combo pill? $60. That’s a 40% discount-sounds fair, right?
- Now replace one brand-name drug with its generic version? The combo still costs $60.
- Buy the generic + the brand-name drug separately? $15.
That’s the “1+1=1.6” rule from IQVIA: combo pills cost about 60% of two brand-name pills-but often 400% more than the sum of their generic parts. It’s not about efficiency. It’s about exploiting gaps in how insurance pays.
Medicare Part D pays for combos based on the drug’s list price, not what it actually costs to make. Meanwhile, the VA, which negotiates directly with drugmakers, pays 22-33% less for the exact same pills. So if you’re on Medicare, you’re paying more than a veteran with the same condition.

Who’s paying the bill?
You are. Even if you have insurance, your premiums go up to cover these inflated prices. Pharmacy benefit managers (PBMs) often don’t push for cheaper alternatives because they get kickbacks from drugmakers on branded combos. And when your doctor prescribes a combo, they rarely check if the same drugs are cheaper separately-unless they’ve done the math themselves.
Take Kazano: a combo of alogliptin and metformin. The combo costs $425 a month. Generic metformin? Under $10. Even if you had to pay full price for the alogliptin (which is still cheaper than the combo), you’d save hundreds. But most patients never know this. Pharmacists don’t always flag it. And insurers don’t force the issue-until it’s too late.
When combos actually make sense
Not all combos are bad. For HIV patients, taking one pill instead of five can boost adherence by 15-20%. That means fewer hospital visits, fewer complications, lower long-term costs. For elderly patients with multiple conditions, reducing pill burden can prevent missed doses and dangerous interactions.
But here’s the key: those benefits should be weighed against cost. A combo that costs $500 a month isn’t “better” if a $25 alternative works just as well. The American College of Cardiology says combos can improve adherence by 25% in certain groups-but only if they’re affordable. If a patient skips their meds because they can’t afford the combo, the “adherence benefit” vanishes.
Real-world data from the University of Michigan Health System shows that switching patients from expensive combos to separate generics saves about $1,200 per person per year. That’s not just a win for the system-it’s a win for the patient’s wallet.
What you can do right now
If you’re on a combo drug, ask your pharmacist or doctor this:
- Are both ingredients available as generics?
- What’s the cash price for each generic separately?
- Can I take them at the same time? (Most can.)
- Will my insurance cover the separate generics?
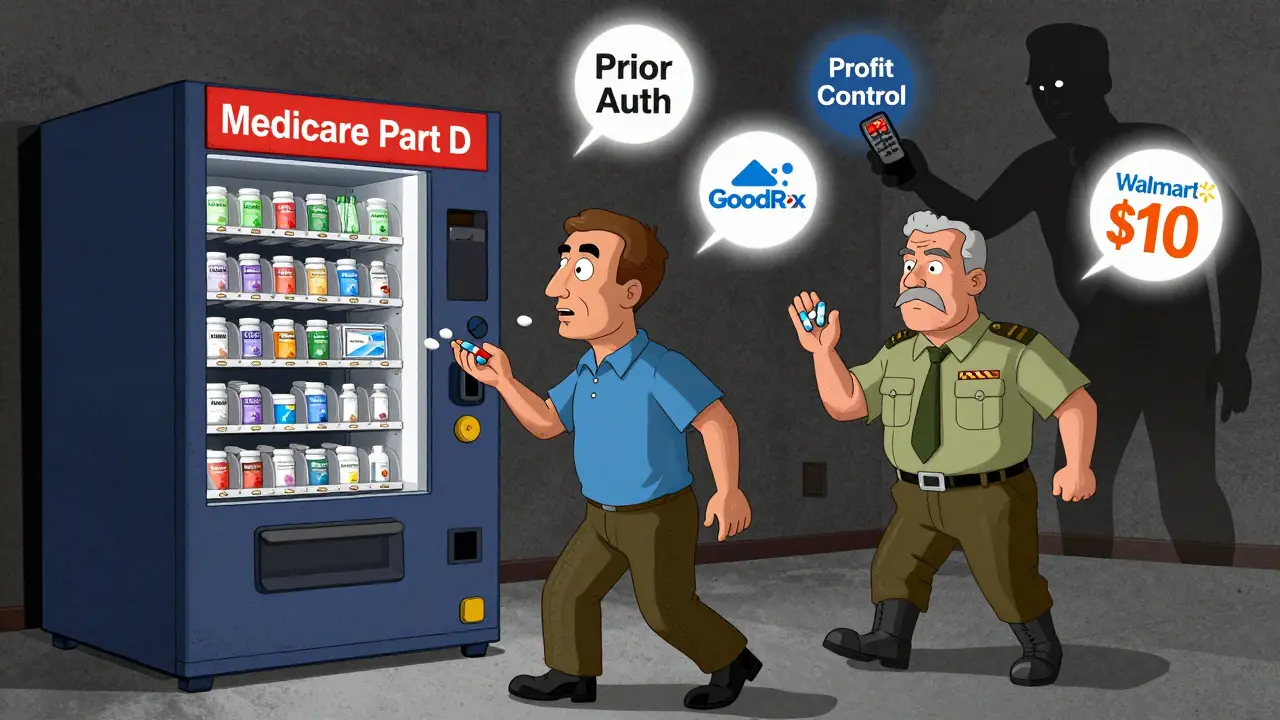
Use tools like GoodRx or SingleCare to compare prices. At Walmart, Target, or Costco, many generics cost under $10 a month. You might be paying $400 for a pill that could be $25.
Some insurers now have “preferred generic” policies that cover separate generics with low or no copay. Others require prior authorization for combos-meaning you have to prove you’ve tried cheaper options first. If your plan doesn’t, ask them why.
Why the system won’t fix itself
Drugmakers argue combos improve health outcomes. They’re not wrong-but they’re not telling the whole story. The real issue isn’t adherence. It’s pricing. The Inflation Reduction Act of 2022 gave Medicare power to negotiate prices for high-cost drugs. But combo pills? They’re still mostly excluded. The FDA is speeding up generic approvals, but that doesn’t help if the combo stays priced like a luxury item.
Companies like Novartis offer co-pay cards for Entresto, lowering it to $10 a month. Sounds great-until you realize the generic version of valsartan (one of its two ingredients) costs $5. The card doesn’t fix the system. It just makes the overcharge feel less painful.
What’s next?
Medicare is projected to spend $14.3 billion more on branded combos than on generic alternatives between now and 2032. That’s money that could go to nursing care, mental health services, or lowering premiums. The Congressional Budget Office says the gap is growing, not shrinking.
But change is possible. When patients ask for cheaper options, when pharmacists push back, when doctors start prescribing separately-it adds up. In 2026, you have more power than you think. You don’t have to accept the price on the label. You just have to ask.
Are combo pills always more expensive than buying generics separately?
Not always-but in most cases where one or both ingredients are generic, yes. If both drugs in the combo are still under patent, the combo might be cheaper than buying two brand-name pills. But if one is generic (like metformin or valsartan), the combo will almost always cost far more than buying the two separately. The difference can be 10x or more.
Can I split my combo pill and take the generics separately?
You don’t need to split anything. You can ask your doctor to prescribe the two generic drugs separately. Most combination pills are just two pills in one shell-they’re not chemically fused. Taking them as two separate pills at the same time works just as well. The only exception is if the combo uses a special timed-release formula that can’t be duplicated with separate pills. That’s rare.
Why don’t doctors know about this cost difference?
Many don’t. Drug reps promote combos because they’re profitable. Electronic health records often default to prescribing combos. And most doctors don’t have time to check cash prices for every medication. But it’s changing. More clinics now use tools that flag high-cost combos and suggest cheaper alternatives. If you ask, your doctor can look it up in seconds.
Will my insurance cover the separate generics?
Usually, yes. Most plans cover generics at low copays-often $5 or less. Some even have $0 copays for certain drugs. Check your plan’s formulary or call customer service. If your plan denies coverage, ask for a prior authorization form. Many insurers will approve the separate generics if you show the combo is much more expensive.
Is it safe to switch from a combo to separate generics?
Yes, if your doctor approves it. The active ingredients are identical. The only difference is how they’re packaged. Many patients switch successfully. Some prefer the combo for convenience, but if cost is a barrier, switching to generics is not just safe-it’s often smarter. Just make sure you’re taking the right doses and timing. Your pharmacist can help you set up a routine.

I had no idea combo pills cost this much. I’ve been taking one for my BP and sugar and just assumed it was cheaper. Just checked GoodRx-my combo is $420, but the two generics are $12 total. Holy crap. I’m switching tomorrow.
This is an egregious exploitation of the healthcare system-and it’s not even remotely defensible. Drug manufacturers are engaging in predatory pricing under the guise of ‘convenience,’ while patients, especially the elderly and those on fixed incomes, are being financially devastated. The FDA and CMS are complicit in this fraud.