Medication Preferences Tool
This tool helps you clarify your medication preferences for your medical power of attorney. The more specific you are, the better your agent can make decisions when you can't speak for yourself.
Pain Management
How do you want to handle pain when you can't communicate?
Antibiotics
What are your preferences about antibiotics?
Blood Thinners
How do you feel about blood thinners?
Psychiatric Medications
What are your thoughts on psychiatric medications?
Other Medications
Any other important medication preferences?
Your Medication Preferences
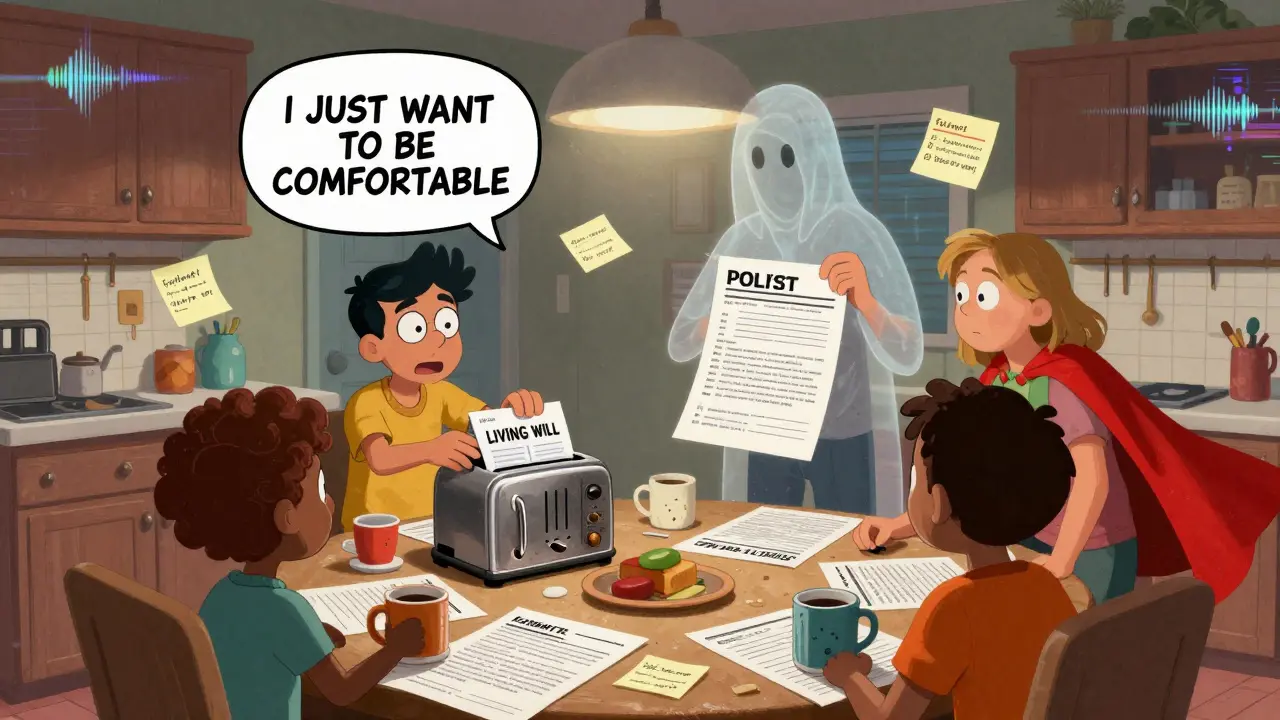
Imagine you’re in the hospital after a stroke. You can’t speak. The doctors ask your family: Should we give her the blood thinner? What about the pain meds? Should we keep her on antibiotics? But no one knows what you’d want. That’s not a hypothetical. It happens every day. And it’s avoidable.
A medical power of attorney isn’t just paperwork. It’s a lifeline for your care when you can’t speak for yourself - especially when it comes to medication. It lets someone you trust make decisions about what drugs you get, how you get them, and when to say no. And it’s not just for older people. Accidents, sudden illness, or dementia can happen at any age.
What Exactly Is a Medical Power of Attorney?
A medical power of attorney (also called a healthcare proxy or durable power of attorney for health care) is a legal document that names a person - your agent - to make medical decisions for you if you’re unable to. It doesn’t take effect until you’re unconscious, too confused, or otherwise unable to communicate. Until then, you’re still in charge.
This document gives your agent authority over things like:
- Whether to admit or discharge you from a hospital or nursing home
- Which medications to give - including painkillers, antibiotics, blood thinners, or psychiatric drugs
- Whether to allow injections, IVs, or oral pills
- Access to your medical records
- Life-sustaining treatments, including feeding tubes or ventilators
All 50 U.S. states recognize this document. But rules vary. In some places, you need two witnesses. In others, it must be notarized. A few states require your doctor to sign off if psychiatric decisions are involved. The key? Don’t assume your state’s form is the same as your neighbor’s. Use your state’s official form.
Why Medication Decisions Are the Most Common Point of Conflict
Studies show that the biggest fights in ICUs aren’t about machines or surgery - they’re about drugs. A 2022 study in the Journal of Medical Ethics found that medication decisions cause more family and medical team conflict than any other issue in critical care.
Why? Because medication choices are nuanced. A painkiller might help comfort, but could also lower breathing. An antibiotic might save a life, but cause severe side effects. A blood thinner could prevent a stroke - or cause internal bleeding.
Without clear instructions, your agent might guess. And guesses often go wrong. A 2023 study in the Journal of Pain and Symptom Management found that patients with a healthcare proxy had 32% fewer medication-related conflicts. But here’s the catch: only 68% of agents accurately understood their loved one’s true preferences - even when they had the document.
That’s not because they’re bad people. It’s because most people never talk about it in detail.
Living Will vs. Medical Power of Attorney: Which One Do You Need?
Many people confuse a living will with a medical power of attorney. They’re different - and you need both.
A living will tells doctors what treatments you want or don’t want in specific situations - like if you’re in a permanent coma or have terminal cancer. It says: “No ventilator. No feeding tube.” But it’s rigid. What if you get pneumonia? What if you’re in a temporary coma and could recover? A living will doesn’t cover that.
A medical power of attorney gives your agent the flexibility to decide based on what’s happening right now. They can say: “Give her the antibiotics - she always said she didn’t want to die from an infection.” Or: “Don’t give her the strong pain meds - she’s terrified of being dazed.”
Think of it this way: a living will is a set of rules. A medical power of attorney is a trusted person who knows your values and can adapt.
Most experts agree: you need both. But if you can only do one, pick the medical power of attorney. It’s more powerful, more flexible, and covers far more real-life scenarios.

How to Choose the Right Agent - And Talk to Them About Medications
Your agent doesn’t have to be your child. Doesn’t have to be your spouse. It should be someone who:
- Knows your values - not just your wishes
- Can stay calm under pressure
- Won’t be easily swayed by other family members
- Is willing to say “no” to doctors if that’s what you’d want
And then - this is critical - you need to talk to them. Not once. Not vaguely. In detail.
Ask yourself: What medications are most important to you?
- Do you want pain meds even if they make you sleepy?
- Would you refuse antibiotics if they meant a longer hospital stay?
- Would you accept a psychiatric drug if it meant you could go home instead of staying in a locked unit?
- Would you rather be comfortable than alive on a ventilator?
Write these down. Share them. Say: “If I can’t speak, I want you to say ‘yes’ to this, and ‘no’ to that.”
One woman in Indiana told her agent: “I don’t want to be drugged into silence. If I’m in pain, give me the morphine. But if I’m just tired and confused, don’t give me the antipsychotics - I hate how they make me feel like a zombie.” When she got septic, her agent remembered that. The hospital wanted to sedate her. Her agent said no. She got pain meds. She went home.
What About POLST? Do You Need That Too?
POLST (Physician Orders for Life-Sustaining Treatment) is a medical order - not a legal document. It’s meant for people with serious, advanced illness. It tells EMS, hospitals, and nursing homes exactly what to do: “No CPR,” “Do not intubate,” “Give antibiotics,” “No tube feeding.”
Unlike a medical power of attorney, POLST is signed by a doctor and becomes part of your medical record. It’s honored across states (in most cases) and travels with you - whether you’re in the ER, at home, or in a nursing facility.
If you’re healthy, you don’t need POLST yet. But if you have a chronic illness - heart failure, COPD, advanced cancer - talk to your doctor about it. POLST and your medical power of attorney work together. One is your voice now. The other is your doctor’s order later.
Common Mistakes - And How to Avoid Them
Most people who fill out these forms never get the outcome they want. Why? Because they make these mistakes:
- They don’t talk to their agent. The form sits in a drawer. The agent has no idea what you’d want.
- They use vague language. “I don’t want to be a burden.” That doesn’t tell your agent whether to give you antibiotics.
- They don’t update it. Your views change. After a diagnosis. After a death in the family. After a hospital stay.
- They assume family will agree. One sibling wants everything done. Another wants comfort only. Without a clear agent and clear instructions, chaos follows.
Fix this: Have the conversation. Write down your specific medication preferences. Give your agent a copy. Tell your doctor. Put a copy in your phone’s health app. Update it every year - or after any major health change.
Where to Get the Right Form - And What It Costs
You don’t need a lawyer. Most states offer free, official forms online.
- California: California Department of Public Health
- New York: NY State Department of Health
- Indiana: Indiana Health Care Quality Resource Center
- Ohio: OhioHealth Advance Care Planning
Some sites offer digital tools like PREPARE (free, from UCSF) that use short videos to help you think through your choices. One study found people who used PREPARE were 43% more likely to complete their forms than those who used paper.
There are paid services - DocuBank, Everplans - that store your documents and send them to hospitals automatically. But they’re not necessary. Free forms work fine if you do the work: talk, write, share, update.
What Happens If You Don’t Do Anything?
If you don’t name an agent and don’t have a living will, the law steps in. In most states, your spouse, adult children, or parents become your decision-makers - in a fixed order. But they may not know you. They may disagree. They may choose based on guilt, fear, or what they think you’d want - not what you actually said.
One man in Pennsylvania died after a family fight over whether to give him blood thinners. His daughter thought he’d want everything done. His son thought he’d want peace. The doctors waited. He had a second stroke. He didn’t survive.
That’s not just tragedy. It’s preventable.
Start Today - Before You Need It
You don’t need to be sick. You don’t need to be old. You just need to be smart.
Take 20 minutes. Download your state’s form. Pick your agent. Talk to them - about pain meds, antibiotics, sedatives, and what matters most to you. Write it down. Give copies to your agent, your doctor, and someone you trust.
Then do it again next year. Or after your next doctor’s visit. Or after your mother’s funeral. Or after your own diagnosis.
Because the goal isn’t just to have a document. It’s to make sure your voice is heard - even when you can’t speak.
