Anticoagulant Timing Calculator
Before Surgery
Calculate when to stop your blood thinner before surgery to minimize bleeding and clotting risks
Why Stopping Blood Thinners Before Surgery Isn’t as Simple as It Sounds
When you’re on a blood thinner-whether it’s warfarin, apixaban, or rivaroxaban-your body is constantly walking a tightrope. Stop it too soon before surgery, and you risk a deadly clot. Keep it too long, and you could bleed out on the operating table. This isn’t theoretical. In 2024, the American College of Cardiology reported that 17-23% of patients on DOACs who had emergency surgery experienced major bleeding. At the same time, 7-16% developed a dangerous clot after stopping their medication. The goal isn’t to eliminate risk. It’s to manage it with precision.
DOACs vs. Warfarin: Two Different Rules for Stopping
Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran changed everything. Unlike warfarin, which takes days to clear from your system and requires regular blood tests, DOACs leave your body quickly. That means you don’t need to bridge with heparin in most cases. The 2023 CHEST guidelines now say: don’t bridge for DOACs unless you have a mechanical heart valve or a recent clot.
Here’s how timing breaks down:
- Apixaban, rivaroxaban, edoxaban: Stop 3 days before surgery
- Dabigatran: Stop 4 days before surgery (longer if you have kidney issues)
- Warfarin: Stop 5 days before surgery, check INR to make sure it’s below 1.5
These aren’t guesses. They come from the PAUSE study, which tracked over 3,000 patients and found that stopping DOACs just 1-3 days before surgery was safe for most elective procedures. No heparin. No extra shots. Just timing.
When You Can’t Stop at All: Low-Risk Procedures
Not every surgery requires you to stop your blood thinner. For minor procedures with little bleeding risk, you can often keep taking it. Think cataract surgery, dental work, or skin biopsies. The 2023 AAFP guidelines confirm that continuing anticoagulants during these procedures doesn’t increase bleeding risk enough to justify stopping.
Why? Because the body’s natural clotting system can still work around the medication in low-trauma settings. Stopping unnecessarily puts you at risk for stroke or pulmonary embolism-especially if you have atrial fibrillation and a CHA2DS2-VASc score of 2 or higher. In those cases, the risk of a clot during a 3-day pause is less than 0.1%. But if you stop and then restart late? That risk jumps.
Resuming Anticoagulants After Surgery: Timing Matters Just as Much
Stopping is only half the battle. Restarting too early can cause internal bleeding. Too late, and you risk a clot forming in your leg or lungs. The standard now is to wait at least 24 hours after surgery before restarting, but the exact day depends on how risky the procedure was.
- Low bleeding risk: Restart DOACs on day 1 after surgery
- High bleeding risk: Wait until day 2 or 3 (e.g., after brain, spinal, or major joint surgery)
For warfarin, restart 12-24 hours after surgery if bleeding is controlled. You’ll need an INR check within 24-48 hours to make sure you’re back in range. DOACs don’t need blood tests, but you still need to follow the timing. Don’t skip the first dose just because you’re still in the hospital. That’s when clots are most likely to form.
Neuraxial Anesthesia: The One Case Where Timing Is Non-Negotiable
If you’re getting an epidural or spinal block, the rules get stricter. A spinal hematoma-bleeding around your spinal cord-can cause permanent paralysis. That’s why ASRA guidelines demand exact timing:
- Factor Xa inhibitors (apixaban, rivaroxaban, edoxaban): Stop 3 days before
- Dabigatran: Stop 4 days before
And you can’t restart until at least 24 hours after the catheter is removed. Even then, if there’s any sign of back pain, weakness, or loss of bladder control, you need an emergency MRI. No exceptions. This isn’t a suggestion. It’s a safety protocol backed by case reports of patients left paralyzed because someone thought “one extra day won’t matter.”
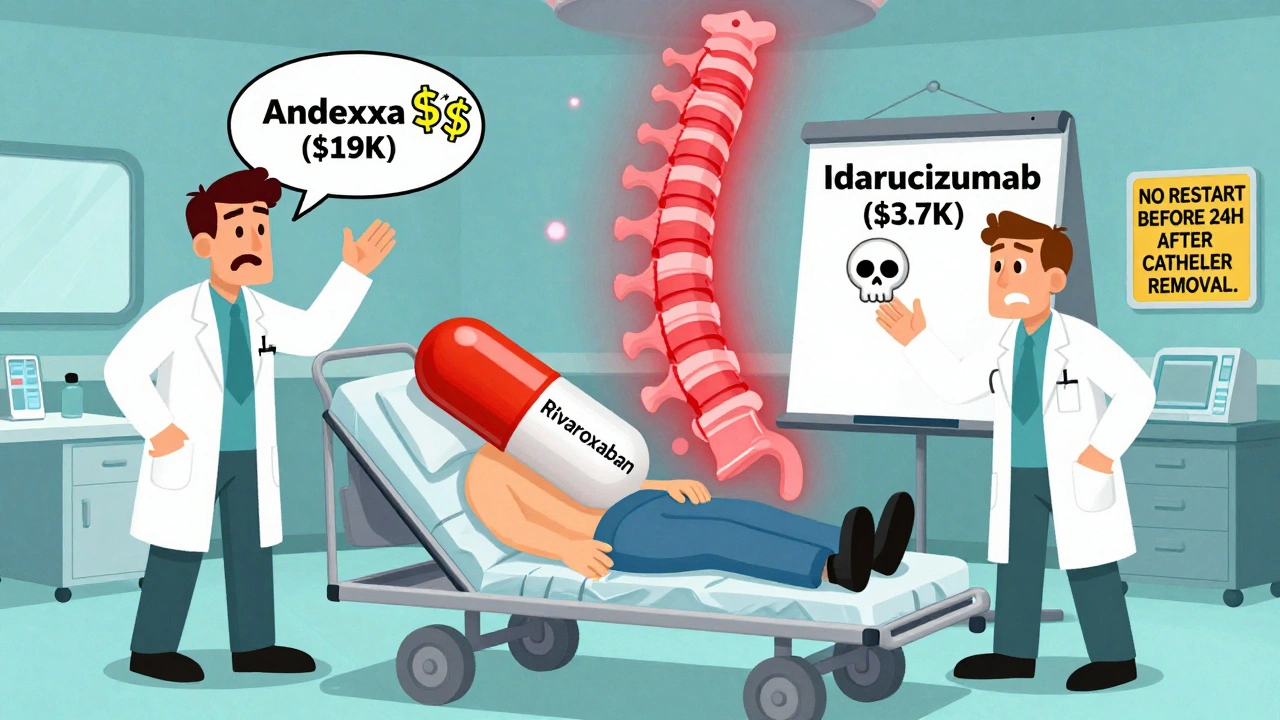
Reversal Agents: What Happens When Things Go Wrong
Emergencies happen. A car crash. A ruptured aneurysm. You need surgery now, and you’re on a blood thinner. That’s when reversal agents come in.
There are two main ones:
- Idarucizumab (Praxbind): Reverses dabigatran in minutes. Costs about $3,700 per vial.
- Andexanet alfa (Andexxa): Reverses apixaban, rivaroxaban, edoxaban. Costs $19,000 per dose.
But here’s the catch: these drugs don’t come without risk. The ANNEXA-4 trial found that 13% of patients who got andexanet alfa had a stroke or heart attack within 30 days. Why? Because once you reverse the anticoagulant, your body’s clotting system goes into overdrive. You’re trading bleeding risk for clot risk.
That’s why reversal agents should only be used in life-threatening bleeding-not for convenience or to speed up surgery. And even then, you need to restart anticoagulation as soon as possible after the bleeding is controlled.
Who Still Needs Heparin Bridging? (Spoiler: Almost No One)
For years, doctors gave patients heparin shots while they stopped warfarin. The idea was to “bridge” the gap. But the evidence is clear now: bridging doesn’t prevent clots. It just causes more bleeding.
ASH 2022 guidelines say: do not bridge for DOACs. And for warfarin? Only consider it if you have:
- A mechanical mitral valve
- A recent clot (within 3 months)
- History of stroke from atrial fibrillation
Even then, the data is mixed. A 2023 study in Annals of Internal Medicine showed that bridging increased major bleeding by 4.5% without reducing stroke risk. For most people with atrial fibrillation, the CHA2DS2-VASc score tells you your stroke risk is low enough that a 3-5 day pause is safe.

Common Mistakes That Put Patients at Risk
Even with clear guidelines, mistakes happen. Here are the top three:
- Misapplying CHA2DS2-VASc or HAS-BLED scores: A 2023 ACC study found 32% of poor decisions came from misusing these tools. Don’t assume “old age” means high stroke risk. Use the actual score.
- Restarting too late: Waiting 5 days after surgery to restart DOACs is common-but dangerous. The highest risk for clots is days 2-4 after surgery.
- Assuming DOAC levels are useful: You can’t test a DOAC level and use it to decide when to operate. No major guideline recommends it. It’s expensive, unreliable, and misleading.
One real case: A 72-year-old man on rivaroxaban had knee replacement. His surgeon stopped the drug 5 days early, didn’t restart it for 7 days, and he developed a pulmonary embolism. He was fine. But he could’ve died. That’s the cost of not following the timeline.
What’s Coming Next: The Future of Anticoagulant Management
The next big thing? Ciraparantag. This experimental drug, currently in Phase 3 trials, could reverse all anticoagulants-including DOACs, heparin, and warfarin-in under 10 minutes. If approved, it could eliminate the need for different reversal agents and make emergency surgeries much safer.
Also, registries like GARFIELD-AF, which tracks over 75,000 patients worldwide, are giving us real-world data on how patients do after surgery while on anticoagulants. That’s helping refine the guidelines even further.
But here’s the truth: the core principles won’t change. It’s still about balancing bleeding and clotting risks. The tools just keep getting better.
What You Should Do Now
If you’re scheduled for surgery and take a blood thinner:
- Don’t stop on your own. Talk to your doctor or anticoagulation clinic.
- Know your drug: Is it a DOAC or warfarin?
- Know your risk: What’s your CHA2DS2-VASc score? Your HAS-BLED score?
- Ask: Do I need to stop? When? When do I restart?
- Write it down. Put it in your phone. Share it with your surgeon.
There’s no one-size-fits-all answer. But there is a clear, evidence-based path. Follow it.
Should I stop my blood thinner before minor surgery like a dental cleaning?
No. For low-bleeding-risk procedures like dental cleanings, cataract surgery, or skin biopsies, current guidelines recommend continuing anticoagulants. Stopping increases your risk of stroke or clot without reducing bleeding risk. Always confirm with your provider, but don’t assume you need to stop.
Can I take aspirin instead of my blood thinner before surgery?
No. Aspirin is not a substitute for anticoagulants like warfarin or DOACs. It doesn’t prevent strokes or clots the same way. Taking aspirin instead could leave you unprotected. Never switch medications without consulting your doctor.
How do I know if I’m at high risk for clots after surgery?
Your risk depends on your medical history. High-risk factors include: recent blood clot (within 3 months), mechanical heart valve, history of stroke from atrial fibrillation, or a CHA2DS2-VASc score of 4 or higher. If you have any of these, your doctor may recommend earlier restart of anticoagulation or short-term bridging-though even that’s rare now.
What if I need emergency surgery and I’m on a DOAC?
If you’re bleeding badly, reversal agents like idarucizumab (for dabigatran) or andexanet alfa (for factor Xa inhibitors) can be used. But these are expensive and carry their own risks-like triggering clots. The priority is stopping the bleeding, then restarting anticoagulation as soon as possible. Hospitals should have protocols in place; tell the ER team you’re on a blood thinner.
Why don’t doctors check DOAC levels before surgery?
Because they’re not useful. Unlike warfarin, DOAC levels don’t reliably predict bleeding risk. Two people with the same drug level can have very different bleeding outcomes. Major guidelines (CHEST, ASH, ACC) all say routine testing isn’t recommended. Timing based on drug type and kidney function is more accurate and simpler.

I had a dental cleaning last month while on apixaban and just kept taking it. No bleeding, no issues. My dentist was surprised but said the guidelines back it up. So glad I didn't panic and stop it myself.
Thanks for this clear breakdown.
You know what they don’t tell you? That the pharmaceutical companies pushed DOACs hard because they make more money than warfarin. The PAUSE study? Funded by the same labs that sell these drugs. And now everyone’s told not to bridge - but what about the patients who *do* clot? They’re just statistics to the guidelines. And don’t get me started on reversal agents costing thousands - it’s a profit scheme disguised as medicine. The system is rigged. We’re all lab rats in a white coat experiment.
Life is a balance. Stop. Restart. Bleed. Clot. We pretend medicine has answers. It just has probabilities.
Wait - so you’re telling me we’re just supposed to ‘trust the timeline’? No labs? No monitoring? No individualization? That’s not medicine - that’s algorithmic dogma. My cousin had a spinal hematoma after they ‘followed the guidelines’ - she’s paralyzed. Now you want me to believe this is safe? You’re not a doctor. I’ve seen what happens when you treat people like numbers.
The body knows what to do. We just interfere too much.
So let me get this straight - you’re saying I can skip the heparin shots, but I still need to remember to restart my pill on day one? That’s the entire medical revolution? We’ve replaced decades of caution with a calendar app?
All these guidelines? Just cover their butts. Real doctors don’t follow them. They listen to the patient. The system’s broken. They don’t care if you live or die - just that they didn’t get sued.
Just a quick note for anyone reading this: if you're on dabigatran and have renal impairment, don't just go by the ‘4 days’ rule - adjust based on eGFR. I’ve seen too many patients get hit with delayed bleeding because someone assumed ‘normal kidney function’ without checking. Also - if you're getting a spinal, always confirm the catheter removal time with your anesthesiologist. That 24-hour window isn't negotiable. And yes, if you’re worried, get the CHA2DS2-VASc score done - it’s free and takes two minutes. Seriously, write it down. Don’t trust your memory.
OMG YES! I’ve been screaming this from the rooftops - DO NOT STOP YOUR MEDS FOR A DENTAL CLEANING! My mom almost had a stroke because her dentist told her to stop warfarin. She’s fine now, but it was terrifying. Thank you for saying what needs to be said - this is life-saving info, not just ‘medical jargon.’ I’m sharing this with my entire book club. 💪❤️