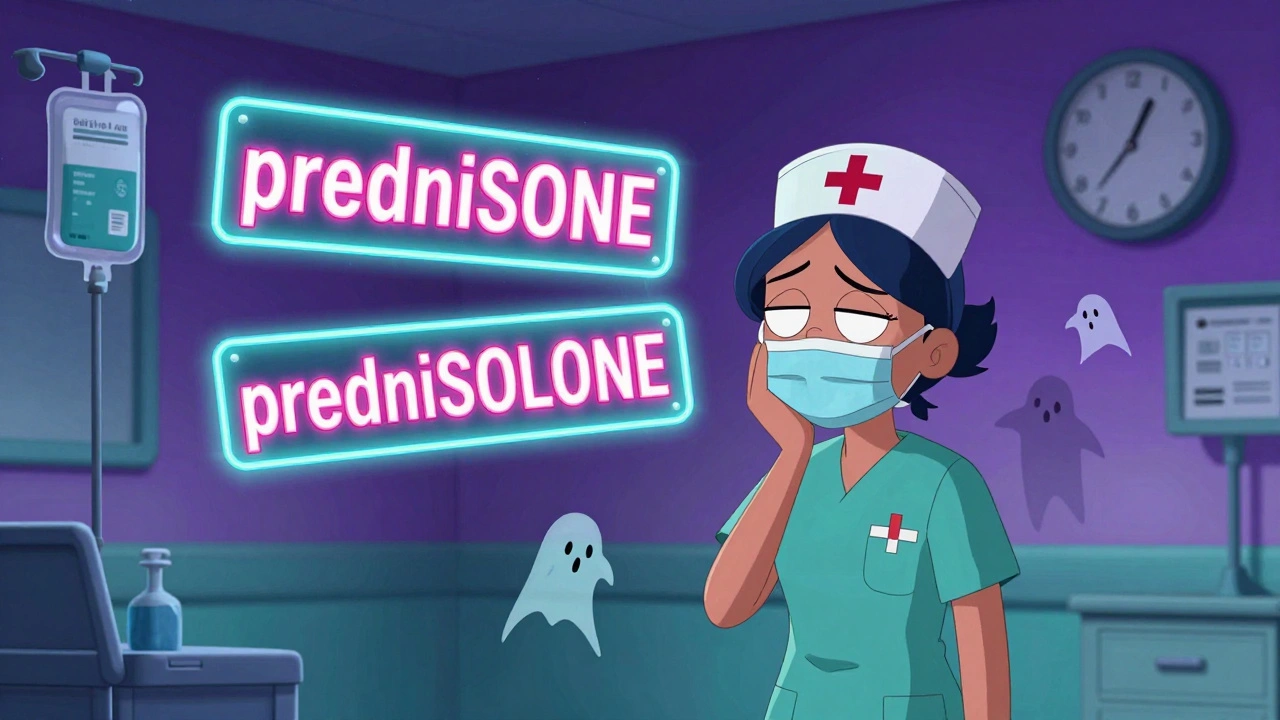
Every year, thousands of medication errors happen because two drug names look or sound too similar. A nurse grabs prednisone instead of prednisolone. A pharmacist dispenses hydromorphone thinking it’s morphine. These aren’t hypothetical mistakes-they’re real, preventable errors that can hurt or even kill patients. The fix? Tall-man lettering.
What Is Tall-Man Lettering?
Tall-man lettering is a simple visual trick: you capitalize the parts of drug names that differ. So instead of writing "prednisone" and "prednisolone," you write "predniSONE" and "predniSOLONE." The uppercase letters jump out, making it easier to spot the difference at a glance.This isn’t just a design choice-it’s a safety tool backed by decades of research. The Institute for Safe Medication Practices (ISMP) introduced the idea in 1999. By 2001, the U.S. Food and Drug Administration (FDA) started officially recommending it. Today, hospitals, pharmacies, and electronic health systems across New Zealand, Australia, and the U.S. use it as a standard practice.
It works because our brains process visual cues faster than text. When you’re tired, rushed, or overwhelmed-like in an emergency room at 3 a.m.-you don’t read every letter. You scan. Tall-man lettering turns a silent, sneaky mistake into an obvious red flag.
How It Works: Real Examples
Not all drug name pairs need the same treatment. The goal is to highlight the part of the name that’s different, not just randomly capitalize letters.
- vinBLAStine vs. vinCRIStine - The "BLA" and "CRI" stand out
- CISplatin vs. CARBOplatin - "CIS" and "CARBO" are the keys
- HYDROmorphone vs. morphINE - "HYDRO" and "INE" are the differentiators
- ALPRAZolam vs. LORazepam - "ALPRA" and "LOR" make the split clear
Notice how the capitalization doesn’t always start at the beginning. It’s about where the difference lies. In "predniSONE" and "predniSOLONE," the difference is in the last four letters. So that’s where the caps go.
Some pairs are trickier. Take "metoprolol" and "methyldopa." Both start with "met," so capitalizing the end doesn’t help. In cases like this, tall-man lettering alone isn’t enough. You need other safeguards-like barcode scanning or double-checks.
Who Uses It and Where?
Tall-man lettering isn’t just on paper labels. It’s built into the systems healthcare workers use every day:
- Electronic health records (EHRs) like Epic and Cerner
- Automated dispensing cabinets (like Pyxis machines)
- Prescription labels and pharmacy packaging
- Barcoding and computerized provider order entry (CPOE) systems
In the U.S., 89% of hospitals use it. In Australia, it’s 76%. New Zealand follows the same standards as Australia, with the National Mixed-Case Lettering List updated regularly. The Joint Commission requires it as part of National Patient Safety Goal NPSG.01.01.01-so if you’re working in a certified hospital, you’re already using it, whether you realize it or not.
But here’s the catch: not everyone uses it the same way.

The Problem: Inconsistent Implementation
Tall-man lettering sounds simple. But in practice, it’s messy.
The FDA, ISMP, and Australia’s safety commission each have slightly different lists. One system might show "PARoxetine," while another shows "parOXETINE." A community pharmacy might use one version, while the hospital’s EHR uses another. Nurses and pharmacists end up second-guessing what they see.
A 2021 ISMP survey found that 63% of pharmacists reported inconsistent tall-man lettering across systems in their own hospital. One pharmacist in Dunedin told me: "I’ve had to pause and check the spelling three times because the system changed the capitalization from yesterday to today. That’s not safety-that’s confusion."
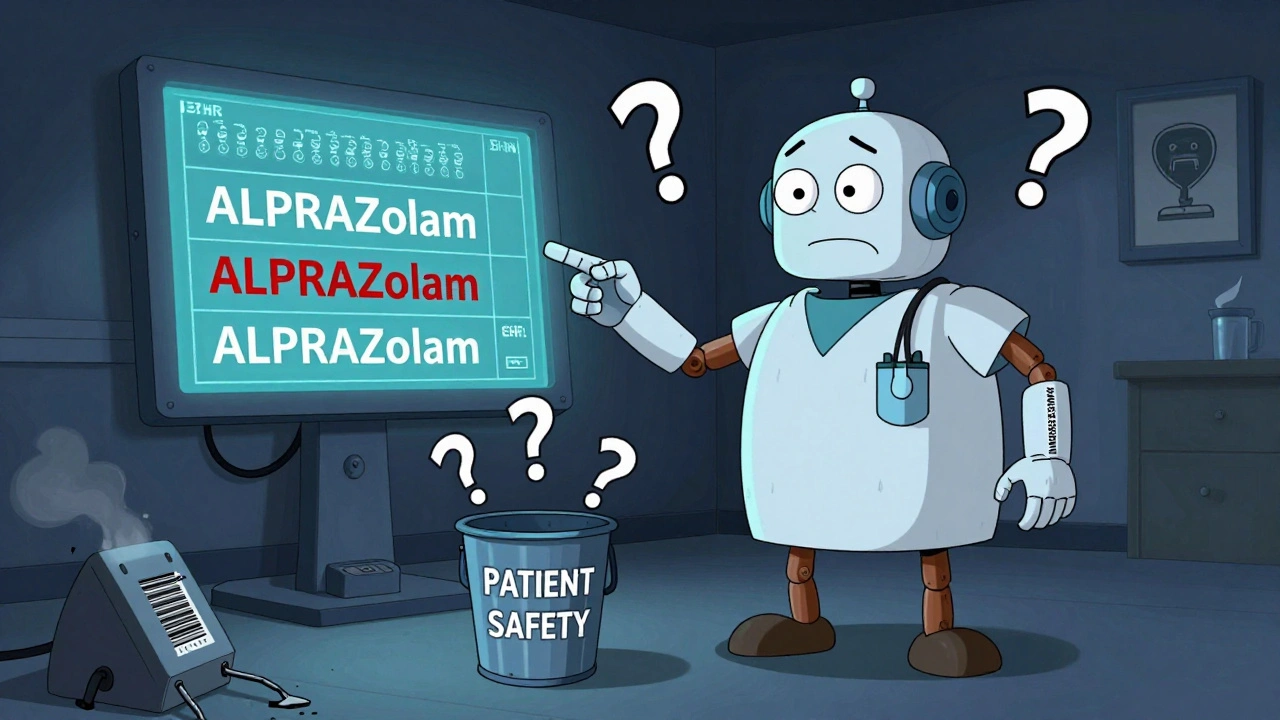
Even worse, some EHR vendors don’t support tall-man lettering properly. Font sizes are too small. The uppercase letters blend in. In a 2022 Reddit thread, a physician wrote: "I keep mixing up ALPRAZolam and LORazepam because our EHR uses a tiny font. The caps are barely visible. I have to zoom in every time. That defeats the whole point."
Does It Actually Work?
Yes-but not always.
A 2004 eye-tracking study by ISMP showed a 35% drop in selection errors when providers used tall-man lettering. In one hospital, after implementing it across 13 systems, they saw a 42% reduction in overridden alerts for look-alike drugs in just six months.
But a 2016 study in Pediatrics found no significant drop in errors. Why? Because they didn’t verify whether the hospitals actually implemented it correctly. The tool only works if it’s applied consistently and clearly.
The Cochrane Collaboration reviewed all the evidence in 2022. Their conclusion? Moderate certainty it reduces selection errors. Low certainty it reduces actual patient harm. That means: it helps you pick the right drug-but it won’t stop every mistake.
That’s why experts don’t call it a silver bullet. Dr. Michael Cohen of ISMP says it’s "one essential layer" in a safety net that includes barcode scanning, independent double-checks, and clear communication.
How to Implement It Right
If you’re setting up tall-man lettering in your system, here’s how to do it right:
- Start with the official lists - Use ISMP’s updated list (252 drug pairs) or your country’s national list. Don’t guess.
- Apply it everywhere - If it’s in the EHR, it must be on the label, the dispensing machine, and the pharmacy database. Inconsistency kills safety.
- Check the font - Use a clear, readable font. Make sure the capitalized letters are bold or slightly larger. Tiny caps in 10-point font are useless.
- Train staff - Don’t assume people know how it works. Show them examples. Run drills. Test them.
- Monitor and adjust - Track error rates before and after. If mistakes don’t drop, look at your implementation. Maybe the capitalization isn’t in the right spot.
Hospitals with over 200 beds typically assign one full-time staff member to manage this. Smaller clinics can share the task, but someone must own it.
What’s Next for Tall-Man Lettering?
The FDA and ISMP are working together to create one unified list by mid-2024. That’s a big step. No more conflicting capitalization between systems.
Some companies are testing AI that adjusts tall-man lettering based on real-time error data. For example, if a certain drug pair keeps being confused, the system could make the difference even more obvious-like making the capital letters blink or highlight in yellow.
But even as automation grows, tall-man lettering isn’t going away. Why? Because humans still make decisions. Screens still glitch. People still get tired. A visual cue that works without needing a login, a scan, or a button press? That’s powerful.
As the Institute for Safe Medication Practices puts it: "Even in highly automated systems, tall-man lettering remains a critical visual safeguard."
What You Can Do Today
You don’t need to wait for a system upgrade to use tall-man lettering.
- If you’re writing prescriptions by hand, use it. Write "HYDROmorphone" and "morphINE."
- If you’re entering orders in an EHR, check if the system uses it. If not, report it.
- If you’re unsure about a drug name, pause. Read it out loud. Compare the capitalized parts.
- Teach new staff. Show them the difference between "CELEcoxib" and "FLOXICin."
Medication safety isn’t about perfect systems. It’s about layers. Tall-man lettering is one of the cheapest, easiest layers you can add. And when it’s done right, it doesn’t just prevent errors-it saves lives.
What is tall-man lettering?
Tall-man lettering is a visual technique that uses selective capitalization in drug names to highlight differences between look-alike, sound-alike (LASA) medications. For example, "predniSONE" and "predniSOLONE" make it easier to distinguish between two similar drugs at a glance, reducing the risk of medication errors.
Which organizations recommend tall-man lettering?
The U.S. Food and Drug Administration (FDA), the Institute for Safe Medication Practices (ISMP), and Australia’s National Mixed-Case Lettering List all officially recommend tall-man lettering. New Zealand follows Australia’s guidelines. These organizations maintain updated lists of drug pairs that require differentiation.
Does tall-man lettering reduce medication errors?
Yes, when implemented correctly. Studies show a 35% reduction in selection errors in controlled settings, and hospitals report up to a 42% drop in overridden alerts after full implementation. However, its effectiveness depends on consistent application across all systems and clear visual formatting. It is not a standalone solution but works best with other safety measures like barcode scanning.
Why do some systems use different capitalization for the same drug?
Different regulatory bodies and EHR vendors have historically used slightly different guidelines. For example, the FDA and ISMP sometimes recommend different capitalization patterns for the same drug pair. This inconsistency creates confusion among staff. A joint FDA-ISMP initiative aims to unify these standards by mid-2024.
Can tall-man lettering be used in small clinics or pharmacies?
Absolutely. Even small clinics can implement tall-man lettering in their prescription labels and electronic systems. The cost is low-often under $1,200 per system-and the benefit is high. The key is consistency: use the same format across all documents, labels, and screens. Staff training and using official lists from ISMP or your national health authority are critical.
What are the limitations of tall-man lettering?
Tall-man lettering doesn’t work well when the difference between drug names is at the beginning (e.g., "metoprolol" vs. "methyldopa"). It also fails if fonts are too small, capitalization is inconsistent, or staff aren’t trained. It’s not a replacement for double-checks, barcode scanning, or clear communication-it’s a visual aid that works best as part of a broader safety strategy.
I worked ER nights for 8 years and I swear tall-man lettering saved my ass more than once. One time I almost gave a patient predniSONE instead of predniSOLONE because I was half-asleep and the font was tiny. After they fixed the EHR system to use bold caps, I stopped second-guessing myself. It’s not magic, but it’s the closest thing we got to a caffeine IV for safety.
Ugh. Another ‘safety’ gimmick. We got AI, barcode scanners, robots… and we’re still capitalizing letters like it’s 2003? 😒
Oh wow, so we’re back to ‘make it look different’ instead of ‘make it actually different’? Classic. In India, we just say the full name out loud and hope the pharmacist doesn’t fall asleep mid-sentence. 😅
so like… uhhh… predniSONE and predniSOLONE? yeah i get it but my eyes glaze over after the 3rd one. also why does my hospital use ALL CAPS for the whole word sometimes?? 🤷♀️
Let’s be real - tall-man lettering is just a band-aid on a systemic failure. The real issue is EHR vendors not standardizing their font rendering, lack of mandatory training, and the fact that 70% of nurses aren’t trained in pharmacology beyond ‘red pill = good’. ISMP’s list is outdated, FDA’s guidelines are inconsistent, and Cerner’s implementation is a joke. If you’re not using the 2023 ISMP update with dynamic font sizing based on screen resolution, you’re doing it wrong. And yes, I’ve audited 12 hospital systems. I know.
Okay but have you SEEN what happens when a pharmacy uses ‘ALPRAZolam’ and the EHR uses ‘alPRAZolam’? I had a coworker cry in the supply closet last week because she almost gave a patient a lethal dose because the capitalization changed overnight. Like… who decides this?? Why is it so chaotic?? I’m not even mad, I’m just… devastated. 🥺
THIS IS SO IMPORTANT!! 💪 Let’s get this into every clinic, every script, every damn label!! 🙌 Tall-man lettering = free safety upgrade. No app download. No training seminar. Just CAPITAL LETTERS. And guess what? It works. I’ve seen it. I’ve used it. I teach my interns. 🏥❤️ #MedSafety #TallManPower
Y’all are overcomplicating it. If the system doesn’t render the caps clearly, it’s not the method’s fault - it’s the vendor’s. Demand better fonts. Demand bold. Demand contrast. If your EHR can’t handle uppercase letters without squishing them into oblivion, it’s time to switch. I’ve been pushing this for 5 years. No more excuses.