Two people walk into a doctor’s office. One is tired all the time, gains weight no matter what she eats, and feels cold even in summer. The other is jittery, losing weight despite eating more, sweating through her clothes, and her heart races for no reason. Both have the same gland acting up - the thyroid. But what’s happening inside them is completely opposite. That’s the core difference between hypothyroidism and hyperthyroidism.
What Your Thyroid Actually Does
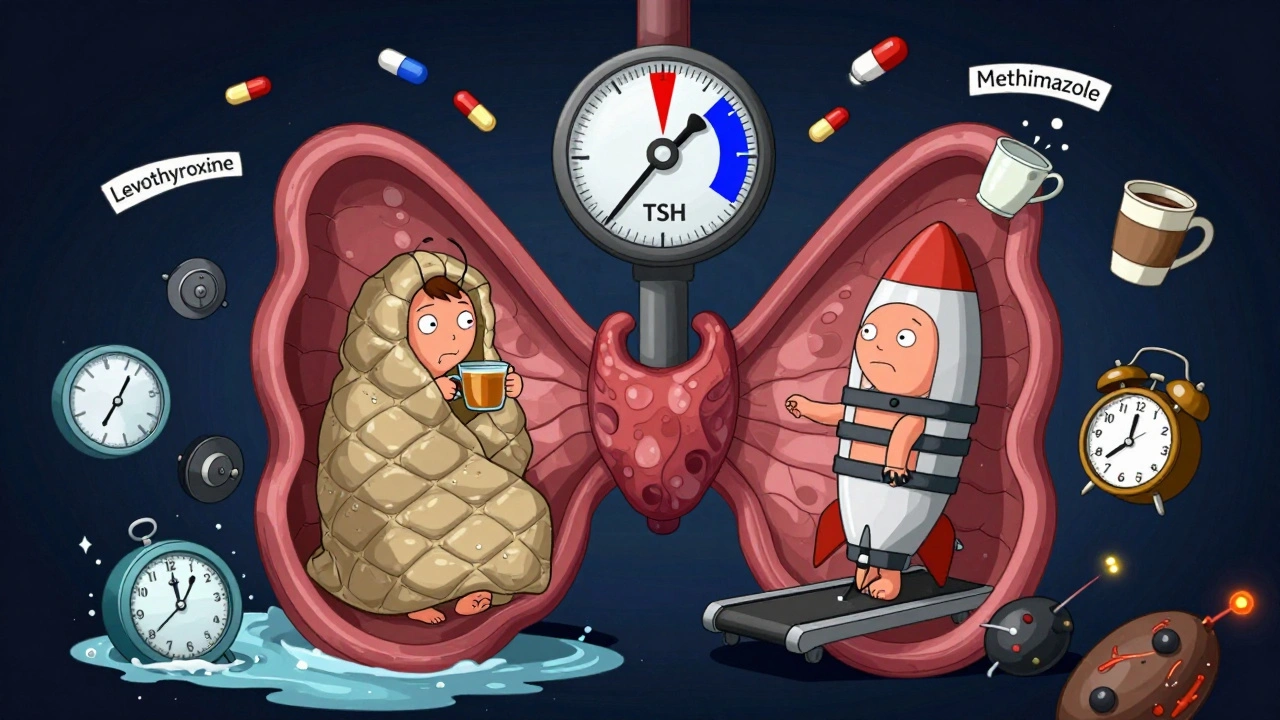
Your thyroid is a small butterfly-shaped gland at the base of your neck. It doesn’t just make hormones - it runs your body’s speed dial. The two main hormones it produces, T4 and T3, tell your cells how fast to burn energy. Too little? Everything slows down. Too much? Everything speeds up. It’s not about being lazy or overworked - it’s biology.
These hormones are controlled by TSH, a signal from your pituitary gland. When T4 and T3 drop, TSH rises to tell the thyroid to produce more. When they’re too high, TSH drops. That feedback loop is simple - until it breaks.
Hypothyroidism: Your Body on Idle
Hypothyroidism means your thyroid isn’t making enough hormones. About 4.6% of U.S. adults have it - and most don’t know it yet. Symptoms creep in slowly. You think you’re just getting older, stressed, or out of shape. But it’s your metabolism stuck in neutral.
- Heart rate drops below 60 beats per minute
- Weight gain of 10-30 pounds, even with no change in diet
- Constant cold - 87% of patients report this
- Dry skin, brittle hair, and hair loss
- Constipation, brain fog, depression
- Heavier, longer periods in women
The #1 cause? Hashimoto’s thyroiditis. That’s when your immune system attacks your thyroid like it’s an invader. It’s autoimmune. It doesn’t just happen overnight - it’s a slow burn. Other causes include thyroid surgery, radiation treatment, or certain medications.
Diagnosis is straightforward: high TSH (above 4.5 mIU/L) and low free T4. But here’s the catch - some people have normal TSH but still feel awful. That’s because not everyone converts T4 to T3 efficiently. About 15% of people have genetic differences that make standard levothyroxine (T4) treatment less effective for them.
Hyperthyroidism: Your Body on Fire
Hyperthyroidism is the opposite. Your thyroid is overproducing. Your body feels like it’s running on 110%. It’s exhausting. It’s scary. And it’s often mistaken for anxiety or a heart problem.
- Heart rate over 100 bpm - sometimes hitting 140 while sitting
- Weight loss despite increased hunger
- Heat intolerance - 89% of patients feel too hot
- Anxiety, panic attacks, trembling hands
- Frequent bowel movements or diarrhea
- Lighter, irregular periods
Graves’ disease causes 70-80% of cases. It’s also autoimmune - but instead of destroying the thyroid, your immune system tricks it into overproducing. Other causes include toxic nodules or multinodular goiters.
Diagnosis? Low TSH (below 0.4 mIU/L) and high free T4 or T3. But there’s a hidden danger: in older adults, hyperthyroidism doesn’t look like the textbook case. Up to 40% of people over 65 show ‘apathetic thyrotoxicosis’ - no jitteriness, no rapid heartbeat. Just fatigue, weight loss, and depression. It looks like dementia. That’s why it’s missed so often.
How They’re Treated - And Why It’s Not the Same
Hypothyroidism treatment? Simple. Take a daily pill: levothyroxine. It replaces the missing T4. Most people feel better in 6-8 weeks. Dose is based on weight - around 1.6 mcg per kg. But timing matters. Take it on an empty stomach, 30-60 minutes before breakfast. Coffee, calcium, iron, or even soy can block absorption. About 45% of people struggle with this - not because they’re forgetful, but because life gets in the way.
For those who still feel off despite normal labs, some doctors add T3 (liothyronine). But it’s not for everyone. Only about 15% of patients have the genetic profile that benefits from combination therapy. The rest? Stick with T4. It works.
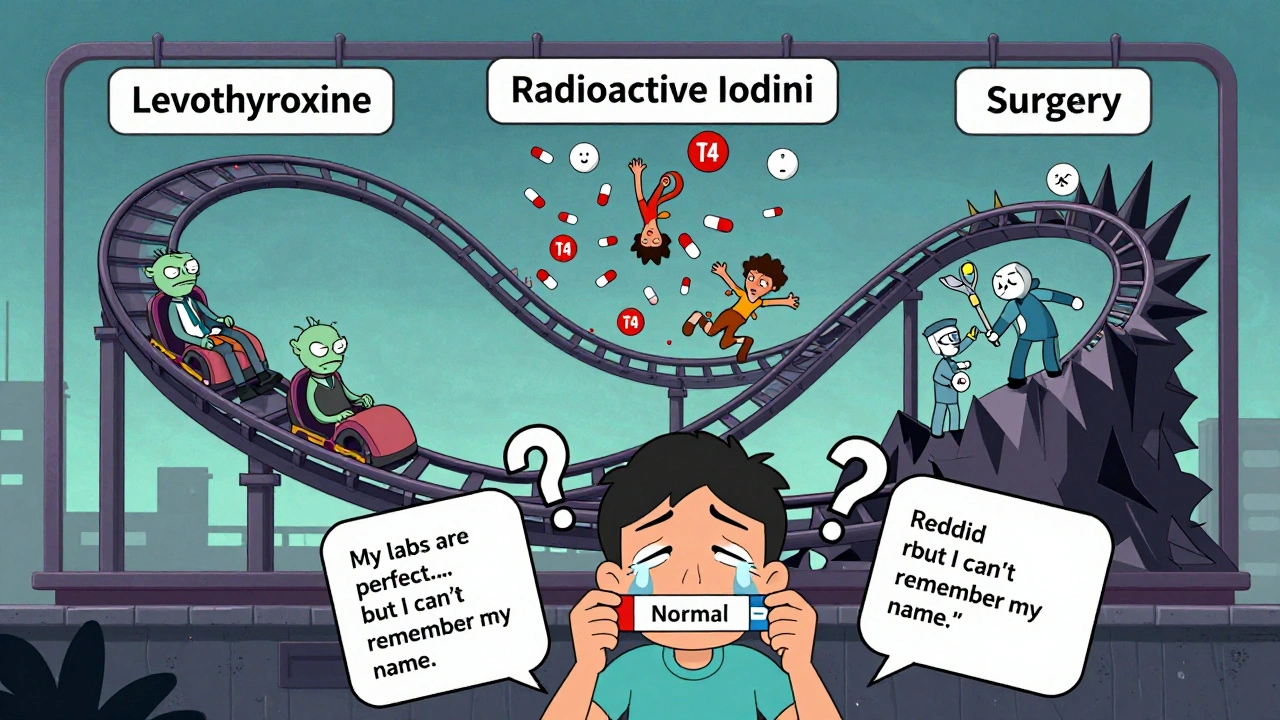
Hyperthyroidism? Three paths - and each has trade-offs.
- Antithyroid drugs: Methimazole (5-60 mg/day) or propylthiouracil (PTU). They block hormone production. But PTU carries a rare but serious liver risk - 1 in 5,000 cases. Methimazole is safer, but can cause low white blood cell counts (1 in 500). Monthly blood tests are needed.
- Radioactive iodine: You swallow a pill. The radiation destroys overactive thyroid tissue. It’s effective - but 80% of people end up with hypothyroidism within a year. That means lifelong levothyroxine. For many, that’s a fair trade. Especially since it’s a one-time treatment.
- Surgery: Removing part or all of the thyroid. Reserved for large goiters, cancer risk, or when other treatments fail. Recovery takes weeks. You’ll need hormone replacement afterward.
Doctors now recommend earlier use of radioactive iodine, even in younger patients. Why? Because long-term drug use is messy. And hypothyroidism is predictable. You know how to fix it.
Why One Is Easier to Manage Than the Other
Hypothyroidism wins on simplicity. One pill. One goal: normalize TSH. 95% of patients respond well. It’s reliable. But it’s not perfect. Poor absorption. Wrong dose. Genetic issues. And the mental toll - feeling broken even when labs look fine - is real. One Reddit user put it: “My doctor says my labs are perfect. But I still can’t remember my own name.”
Hyperthyroidism is trickier. It’s not just about fixing numbers. It’s about stopping a runaway train. Medications have side effects. Radioactive iodine creates a new condition. Surgery has risks. And thyroid storm - a rare but deadly spike in hormone levels - can kill. Mortality is 10-20% if not treated in time.
But here’s the upside: once you treat it - especially with radioactive iodine - you’re done with the chaos. You swap hyperthyroidism for hypothyroidism. And hypothyroidism? You’ve got a solid plan for that.
Who’s Most at Risk?
Women are 5 to 8 times more likely than men to develop either condition. Why? Likely tied to X-chromosome immune factors. About 75-80% of all thyroid cases are in women.
Age matters too. Hypothyroidism hits harder after 50 - 10% of women over 50 have it. Hyperthyroidism has two peaks: 20-40 (Graves’ disease) and 60+ (toxic nodules). And older adults? Their symptoms hide. That’s why screening isn’t just for the young.
Family history? Big red flag. If your mom or sister has Hashimoto’s or Graves’, your risk jumps.
What You Should Do If You Suspect Something’s Off
Don’t wait. Don’t assume it’s stress. Get a TSH test. It’s cheap - $25 to $50. It’s the first and most important step. The American Thyroid Association says TSH screening catches 98% of thyroid disorders.
If your TSH is abnormal, ask for free T4 and free T3. Don’t stop there. If you still feel bad but your labs are “normal,” ask about antibody tests (TPOAb, TgAb) - they can reveal Hashimoto’s or Graves’ even before hormone levels shift.
And if you’re on levothyroxine and still tired? Talk about T3 conversion. Ask if genetic testing for deiodinase enzymes is right for you. It’s not routine - but it’s growing in use.
What’s Changing in 2025
Thyroid care is evolving. The FDA approved selumetinib for thyroid cancer - not for hypothyroidism or hyperthyroidism - but it shows progress in targeted therapies.
New drugs like Resmetirom are in phase III trials. It’s designed for thyroid hormone resistance - a rare condition where cells don’t respond to T3, even when levels are normal. Early results show 65% symptom improvement in 12 weeks.
AI tools are helping doctors spot patterns earlier. One system improved diagnosis accuracy by 22%. And patient education? Studies show people who get clear, structured info have 35% better adherence and 28% fewer ER visits.
The future? Personalized treatment. Not just “take this pill.” But “take this pill, because your genes say you need it.”
Bottom Line
Hypothyroidism and hyperthyroidism are mirror images. One slows you down. The other speeds you up. Both are common. Both are treatable. But they demand different approaches.
If you’re tired, cold, and gaining weight - get tested. If you’re anxious, losing weight, and your heart races - get tested. Don’t let symptoms be dismissed as stress, aging, or anxiety. Thyroid disorders are medical conditions. They don’t go away on their own.
And if you’re already diagnosed? Stick with your treatment. Timing matters. Follow-ups matter. And if something still feels off - speak up. Your body is trying to tell you something. Listen.
Can hypothyroidism turn into hyperthyroidism?
Not directly. Hypothyroidism and hyperthyroidism are different conditions with different causes. But treatment for hyperthyroidism - especially radioactive iodine or surgery - often results in hypothyroidism. That’s not a switch from one to the other; it’s a side effect of treatment. You go from overactive to underactive because the thyroid tissue was destroyed or removed. That’s why most people who get radioactive iodine end up on levothyroxine for life.
Is levothyroxine safe long-term?
Yes, when taken correctly. Levothyroxine is a synthetic version of the T4 hormone your body naturally makes. It’s one of the most prescribed medications in the U.S. - over 114 million prescriptions in 2022. Long-term studies show no increased risk of heart disease, osteoporosis, or cancer when TSH is kept in the normal range. The danger comes from too much or too little. Too much can cause bone loss or irregular heartbeat. Too little leaves you symptomatic. Regular blood tests every 6-12 months keep you on track.
Can diet cure thyroid problems?
No. Diet can’t cure hypothyroidism or hyperthyroidism. But it can support treatment. For example, people with Hashimoto’s often have celiac disease or gluten sensitivity - avoiding gluten may reduce inflammation and improve medication absorption. Iodine is tricky: too little causes hypothyroidism, too much can trigger hyperthyroidism in susceptible people. Most people in the U.S. get enough iodine from iodized salt. Avoid massive doses from supplements unless prescribed. Selenium-rich foods (Brazil nuts, fish) may help reduce thyroid antibodies in Hashimoto’s - but it’s not a cure.
Why do some people still feel bad even with normal TSH?
Because TSH doesn’t tell the whole story. Some people don’t convert T4 to T3 efficiently due to genetic differences in deiodinase enzymes - affecting about 15% of patients. Others have high thyroid antibodies causing ongoing inflammation. Stress, poor sleep, or other hormones like cortisol can interfere too. If you’re still tired, cold, or foggy despite normal labs, ask about free T3, reverse T3, and thyroid antibodies. You’re not imagining it. Your symptoms matter - even if the numbers look fine.
Can you have both conditions at once?
Not at the same time. But some people experience both over their lifetime. For example, someone with Hashimoto’s might go through a phase called “hashitoxicosis” - where damaged thyroid cells leak stored hormones, causing temporary hyperthyroidism. It lasts days or weeks, then the gland burns out and hypothyroidism returns. This isn’t having both conditions - it’s one condition with fluctuating phases. It’s confusing, but common enough that doctors know to watch for it.
Is thyroid cancer linked to these conditions?
Hypothyroidism and hyperthyroidism themselves don’t cause thyroid cancer. But people with thyroid nodules - especially in hyperthyroidism from toxic nodules - have a slightly higher risk. Most nodules are benign. If you have a goiter or lump, your doctor will likely order an ultrasound and maybe a biopsy. The key is monitoring. If your thyroid is enlarged or has irregular nodules, don’t ignore it. Cancer risk is low, but early detection saves lives.

Oh please. Another ‘thyroid is the master gland’ sermon. Newsflash: the hypothalamus is the real puppet master, and your pituitary? Just a glorified relay station. You treat hypothyroidism like it’s a light switch, but it’s a goddamn symphony - and most doctors can’t even tell the difference between a cello and a tuba. Levothyroxine isn’t a cure, it’s a band-aid on a ruptured aorta.
thiroid? more like thyro-idiot. everyone thinks they have it bc they’re tired or ate bread. i had a ‘low tsh’ once. turned out i was just sleep deprived and drunk on matcha. also, ‘reverse t3’? sounds like a crypto coin. lol.
In India, thyroid is common. Many eat too much soy. Too little iodine. Doctors test TSH only. No free T3. No antibodies. People suffer for years. One pill does not fix everything. Culture matters. Diet matters. Sleep matters. Not just labs.
I’ve been on levothyroxine for 7 years. My TSH is ‘perfect.’ My doctor says I’m fine. But I cry in the shower. I forget my kids’ birthdays. I feel like a ghost in my own body. And no one listens. Not even my husband. He says I’m ‘just dramatic.’ Guess what? I’m not dramatic. I’m exhausted. And I’m tired of being told I’m fine when I’m not.
It is an empirical fallacy to conflate symptomatology with biochemical normalization. The diagnostic paradigm currently employed in endocrinology is predicated upon a reductionist model that ignores systemic neuroendocrine dysregulation. Levothyroxine monotherapy, while statistically efficacious in population cohorts, fails to account for interindividual variability in deiodinase polymorphisms, which are non-normatively distributed across the human genome. Ergo, the current standard of care constitutes a form of therapeutic nihilism disguised as evidence-based medicine.
Yo. I get it. TSH is the gatekeeper, but your body’s like a smartphone with a broken charger - the battery (T3) is low even if the plug (TSH) says it’s charging. I was on T4 for 3 years. Felt like a zombie. Then my doc added T3. Boom. I could breathe again. 😌 I’m not a genius, just someone who refused to accept ‘your labs are fine.’ If you’re still tired, cold, or foggy - don’t let them gaslight you. Ask for T3. Ask for antibodies. Ask for help. You’re not broken. Your thyroid just needs a better team.
Hyperthyroidism treatment is a joke. Radioiodine? Just make them hypothyroid and call it a day. Lazy medicine. Why not fix the autoimmune root? Pharma loves lifelong prescriptions. TSH is a proxy. Not a diagnosis. Most docs don’t even know what TPOAb means. They just prescribe and leave. You’re not a patient. You’re a revenue stream.
my mom had thyroid stuff. she took her pill at night with coffee and calcium. no wonder she felt like crap. i told her: take it on empty stomach, wait 30 min, no soy, no milk, no antacids. she did. now she’s actually alive again. 😅 also, brazil nuts. 2 a day. not a cure, but helps. and yes, your doctor is probably rushing you. ask for more tests. they won’t mind. they just forget to ask.