Drug Interaction Checker
Check for Interactions
Risk: 10-20x increased simvastatin levels → Rhabdomyolysis risk
Recommendation: Avoid this combination. Consider alternative statin.
Risk: 5.7x increased torsades de pointes risk
Recommendation: Monitor heart rhythm closely. Consider alternative antibiotics.
Every year, millions of people take multiple medications - some for chronic conditions, others for short-term issues. But what happens when those drugs meet inside your body? Not all combinations are safe. In fact, drug-drug interactions are one of the most common - and preventable - causes of hospital visits, especially among older adults. Understanding how they work isn’t just for doctors. If you’re on more than one prescription, or even take supplements, this matters to you.
What Exactly Is a Drug-Drug Interaction?
A drug-drug interaction (DDI) happens when one medication changes how another works in your body. It’s not always obvious. Sometimes it makes a drug stronger. Other times, it cancels it out. In the worst cases, it causes dangerous side effects you didn’t expect. There are two main types: pharmacokinetic and pharmacodynamic. Think of pharmacokinetic as what your body does to the drug - how it absorbs, moves around, breaks down, or gets rid of it. Pharmacodynamic is what the drug does to your body - how it affects your cells, organs, or systems when it’s already there.Pharmacokinetic Interactions: The Body’s Drug Transport System
Your body has a system for handling drugs like a delivery network. It absorbs them in the gut, carries them through the blood, breaks them down mostly in the liver, and flushes them out via the kidneys. One drug can mess with any step in this chain. Metabolism is the biggest player. About 70-80% of all clinically important DDIs involve the cytochrome P450 enzyme system - especially CYP3A4, CYP2D6, and CYP2C9. These enzymes act like molecular scissors, cutting drugs into pieces so your body can remove them. If Drug A blocks CYP3A4 (an inhibitor), Drug B - which relies on that enzyme - builds up in your blood. Take simvastatin (a cholesterol drug) with ketoconazole (an antifungal). Ketoconazole shuts down CYP3A4. Simvastatin levels can spike 10 to 20 times higher than normal. That’s not just a side effect - it’s a risk of rhabdomyolysis, a condition where muscle tissue breaks down and can damage your kidneys. On the flip side, some drugs speed up metabolism. St. John’s Wort, a popular herbal supplement for mild depression, is a strong CYP3A4 inducer. It can slash the levels of cyclosporine (used after organ transplants) by 50-60%. That means your body rejects the new organ because the drug isn’t working anymore. Transporters matter too. Proteins like P-glycoprotein (P-gp) act like bouncers at cell doors, deciding what gets in or out. Verapamil, a heart medication, blocks P-gp. When taken with digoxin (used for heart rhythm), digoxin piles up in the blood. Too much can cause deadly heart arrhythmias.Pharmacodynamic Interactions: When Drugs Team Up - or Fight
These don’t change drug levels. They change what the drugs do when they’re already there. Synergistic interactions make effects stronger. Take two drugs that both slow your heart rate - like beta-blockers and calcium channel blockers. Together, they can drop your heart rate dangerously low. Antagonistic interactions cancel each other out. If you’re on a blood pressure pill and take a decongestant like pseudoephedrine, the decongestant can undo the blood pressure control. One of the most dangerous synergistic pairs is fluoroquinolone antibiotics (like ciprofloxacin) with macrolides (like azithromycin). Both can prolong the QT interval - the time your heart takes to recharge between beats. Together, they raise the risk of torsades de pointes, a chaotic heart rhythm that can kill you. Studies show this combo increases that risk by 5.7 times compared to either drug alone. Another classic: ACE inhibitors (like lisinopril) plus potassium-sparing diuretics (like amiloride). Both raise potassium. Together, they can push levels up by 1.0-1.5 mmol/L. High potassium can stop your heart. It’s silent - no symptoms until it’s too late.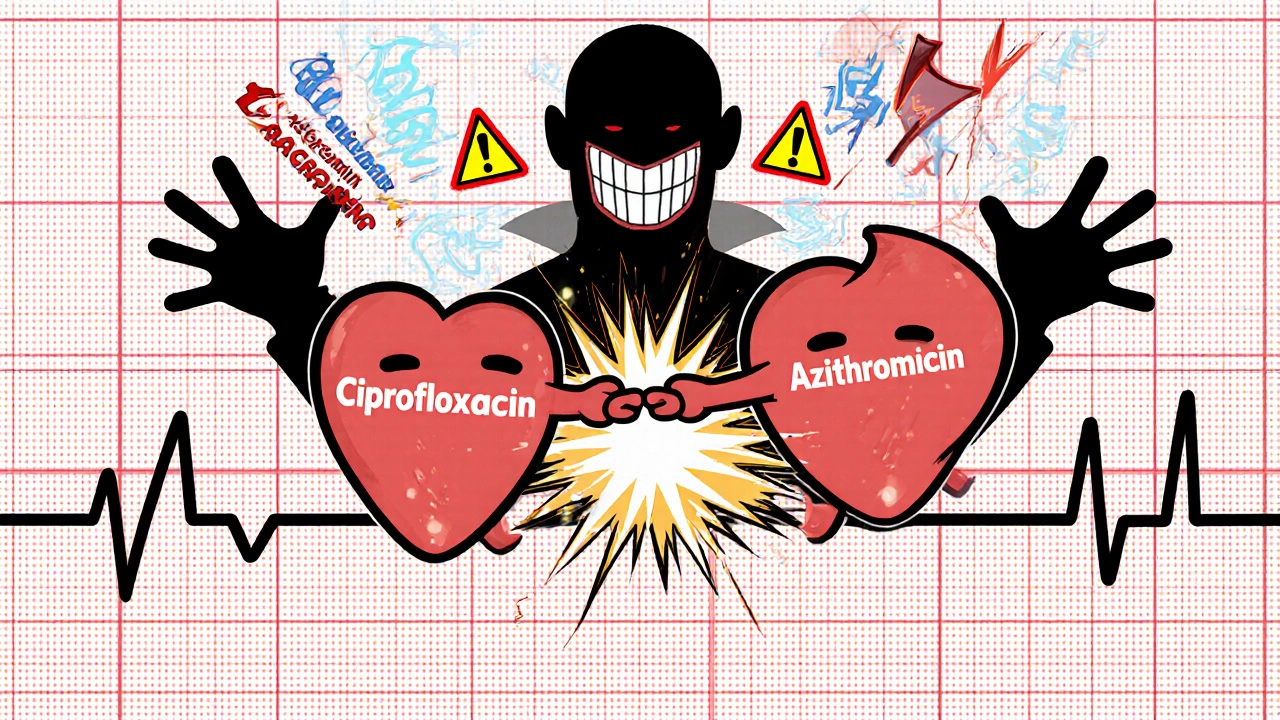
Who’s at Highest Risk?
It’s not random. People taking five or more medications - common in older adults - are most vulnerable. About 3-5% of hospital admissions in people over 65 are due to DDIs. The Beers Criteria, updated in 2019, lists 30 high-risk combinations for seniors. One of the top ones? NSAIDs (like ibuprofen) with blood thinners like warfarin. Together, they triple or quadruple the risk of internal bleeding. Genetics also play a role. Some people are “poor metabolizers” of CYP2D6 - meaning their bodies can’t process certain drugs at all. Codeine, for example, needs CYP2D6 to turn into morphine. In poor metabolizers, it doesn’t work. In ultrarapid metabolizers, it turns into too much morphine too fast - especially dangerous if they’re also taking CYP3A4 inhibitors like clarithromycin.How Are These Interactions Found?
Drug companies test for DDIs before a drug hits the market. They start in labs - using liver cells and enzymes to see if a new drug inhibits or induces CYP enzymes. If the risk looks real, they move to human trials. Healthy volunteers take the new drug with a known “probe” drug to measure changes in blood levels. Regulators like the FDA and EMA require this testing. They use specific thresholds: if a drug raises another’s concentration by more than 5-fold, it’s labeled a “strong” inhibitor. A 2-5-fold increase? “Moderate.” Even small changes matter if the drug has a narrow therapeutic window - meaning the difference between a helpful dose and a toxic one is tiny. Warfarin is a prime example.Real-World Impact: Cost, Hospitalizations, and Alerts That Don’t Work
Preventable DDIs cost the U.S. healthcare system about $1.3 billion a year. Most of that comes from hospital stays for bleeding, kidney failure, or heart problems caused by interactions. Electronic health records (EHRs) are supposed to help. They flash alerts when a doctor prescribes a risky combo. But here’s the problem: 80-90% of those alerts are false or low-risk. Doctors get so used to clicking “ignore,” they stop paying attention. One study found clinicians override 49-96% of DDI alerts. Newer systems are smarter. Epic’s “Suggestive Warnings” feature doesn’t just say “warning.” It says, “This combo increases bleeding risk by 3.5x. Consider switching to acetaminophen.” That reduced serious DDIs by 22% in a study of 4.7 million patients.
What Can You Do?
You don’t need to be a pharmacologist to protect yourself.- Keep a list of everything you take - prescriptions, OTC meds, vitamins, herbs. Even “natural” supplements like St. John’s Wort or garlic pills can interact.
- Ask your pharmacist every time you pick up a new prescription. Pharmacists reviewed 12,543 patients in one study and cut serious DDIs by 37% just by talking to people.
- Use trusted tools. The Liverpool HIV-Drug Interactions Checker updates daily and covers over 350 combinations. Even if you’re not HIV-positive, it’s a good model for how reliable DDI databases should work.
- Watch for symptoms. Unexplained bruising, muscle pain, dizziness, irregular heartbeat, or extreme fatigue could be a sign. Don’t assume it’s “just aging.”
The Future: Personalized Medicine and AI
We’re moving beyond one-size-fits-all warnings. Pharmacogenomics - testing your genes to see how you metabolize drugs - is becoming part of routine care. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has issued 22 guidelines, including advice to avoid codeine in ultrarapid metabolizers, especially if they’re on other drugs that slow its breakdown. Artificial intelligence is catching up fast. One 2021 study trained a machine learning model on 89 million electronic health records. It predicted DDIs with 94.8% accuracy - far better than old rule-based systems. Soon, your doctor might get a real-time alert: “Patient X has CYP2C19 poor metabolizer status and is being prescribed clopidogrel. This combo is ineffective. Switch to prasugrel.”Bottom Line: Knowledge Is Your Shield
Drug-drug interactions aren’t rare accidents. They’re predictable, preventable, and often invisible. Whether you’re managing high blood pressure, diabetes, depression, or just taking a few pills for pain, you’re at risk if you don’t know what you’re mixing. The science is complex. But the solution is simple: know what you’re taking. Talk to your pharmacist. Ask your doctor: “Could this interact with anything else I’m on?” Don’t wait for a hospital visit to learn the answer.Can over-the-counter drugs cause dangerous interactions?
Yes. Common OTC meds like ibuprofen, naproxen, and even antacids can interact. Ibuprofen with warfarin increases bleeding risk. Antacids can block absorption of antibiotics like ciprofloxacin. Even herbal supplements like St. John’s Wort can make birth control, antidepressants, or transplant drugs stop working. Always check with your pharmacist before starting any new OTC product.
Are drug interactions more dangerous for older adults?
Yes. Older adults are more likely to take multiple medications, have reduced liver and kidney function, and experience changes in body composition that affect how drugs are distributed. The Beers Criteria lists 30 high-risk combinations specifically for people over 65. Medications like NSAIDs with anticoagulants, or benzodiazepines with opioids, are especially risky in this group.
Can food or drinks affect drug interactions?
Absolutely. Grapefruit juice blocks CYP3A4 and can double or triple levels of statins, blood pressure drugs, and immunosuppressants. Vitamin K-rich foods like kale and spinach can reduce the effect of warfarin. Alcohol can worsen liver damage from acetaminophen and increase drowsiness from sedatives. Always ask about food and drink interactions when you get a new prescription.
Why do some drug interactions take days to show up?
Because some interactions are slow. Inducers like St. John’s Wort take 1-2 weeks to ramp up enzyme production. Inhibitors like ketoconazole can cause immediate spikes, but others build up gradually. Also, some drugs accumulate over time - like digoxin - so effects appear only after days or weeks of use. Don’t assume no symptoms means no interaction.
How do I know if my meds are interacting right now?
Watch for new or worsening symptoms after starting a new drug: unexplained bruising, muscle pain, dizziness, confusion, irregular heartbeat, nausea, or extreme fatigue. If you notice any of these, don’t ignore them. Bring your full medication list to your doctor or pharmacist. Blood tests (like INR for warfarin or potassium levels) can also reveal hidden interactions.

I had no idea grapefruit juice could mess with my blood pressure med like that. I drink it every morning and just assumed it was harmless. Guess I’m buying orange juice from now on.
This is one of the clearest explanations of drug interactions I’ve ever read. Thank you for breaking down complex pharmacology into something actionable. Everyone on multiple medications should read this.
People who take ‘natural’ supplements are just asking for trouble. St. John’s Wort isn’t a ‘herbal remedy’-it’s a dangerous chemical that shouldn’t be sold over the counter. If you’re dumb enough to mix it with your antidepressants, you deserve what you get.
Wow. Just… wow. The CYP3A4 system? P-glycoprotein? This is the kind of biochemical ballet that makes me feel like a caveman holding a smartphone. I’m not just on meds-I’m in a high-stakes, molecular tug-of-war. And I didn’t even know I was playing! 🤯
It’s fascinating how much we rely on systems we don’t understand-our bodies, our medications, even our healthcare alerts. The fact that doctors ignore 90% of warnings says more about our system than about the science. Maybe we need fewer alerts and more conversations.
Let me drop some real talk: if you’re on more than three meds and haven’t had a pharmacogenomic test, you’re basically rolling the dice with your life. CYP2D6 poor metabolizer? You’re not ‘just sensitive’-you’re a walking time bomb. Get tested. Don’t wait for your heart to skip a beat.
I’ve been on warfarin for years and never thought about how kale in my smoothie could mess with it. I always thought it was just about alcohol. This changed how I think about food. I’m going to start keeping a food + med log now.
My grandma took 12 pills a day. She never complained, but she was always tired. Now I wonder if it was just interactions. I’m going to sit down with her pharmacist next week.
India has no idea how dangerous this is. People buy antibiotics and painkillers at the corner shop and mix them with ayurvedic stuff like it’s tea. They get sick and blame the gods. No. It’s the pills.
Thank you for writing this. It’s easy to feel powerless when you’re on multiple medications, but this gives real tools-not fear. Talking to your pharmacist isn’t annoying, it’s essential. And yes, write down everything-even the gummy vitamins.
USA thinks it invented medicine. We have Ayurveda for 5000 years and we still live longer than you. Your drugs are poison wrapped in labels. We don’t need your CYP enzymes to tell us what’s safe.
How can we, as a society, allow such profound biochemical ignorance to persist? The fact that laypeople must self-educate on cytochrome P450 isoforms to avoid fatal polypharmacy is not just a failure of medicine-it is an existential moral collapse of institutional responsibility.
My dad had a near-fatal interaction between his statin and a generic antifungal. He didn’t know they were interacting until he couldn’t walk. Now I make him bring every new pill to the pharmacy with his list. It’s not a hassle-it’s a habit that saves lives.
And that’s why I always ask my pharmacist: ‘What’s the one thing I shouldn’t mix with this?’ They always know. Most doctors don’t even remember half the drugs they prescribe. Pharmacists are the unsung heroes of patient safety.