When you’re on a blood thinner like apixaban, rivaroxaban, or dabigatran, it’s not just about taking your pill every day. The real risk often comes from what else you’re taking - even if it’s something as simple as an over-the-counter painkiller or a heart rhythm medication. Direct Oral Anticoagulants (DOACs) were designed to be simpler than warfarin. No more weekly INR checks. Fewer food restrictions. But that doesn’t mean they’re safe to mix with anything. In fact, DOAC interactions are one of the most overlooked dangers in modern anticoagulant therapy.
Why DOAC Interactions Matter More Than You Think
DOACs - including apixaban, rivaroxaban, dabigatran, edoxaban, and betrixaban - work by blocking specific clotting factors in your blood. Unlike warfarin, which affects vitamin K and has hundreds of known interactions, DOACs have fewer. But that doesn’t mean they’re immune. The problem? Most people on DOACs are older and taking five or more other medications. Heart disease, diabetes, high blood pressure, arthritis - each condition brings its own drugs. And many of those drugs mess with how your body handles DOACs.
Here’s the key: DOACs rely on two main systems to get cleared from your body - the CYP3A4 enzyme and the P-gp transporter. If another drug blocks or speeds up these systems, your DOAC levels can spike or crash. Too high? Risk of serious bleeding. Too low? Risk of stroke or blood clots. And unlike warfarin, you can’t just check a blood test to see if it’s working right.
Which Drugs Are the Biggest Risks?
Not all interactions are created equal. Some are minor. Others can be life-threatening. The biggest red flags come from drugs that strongly affect CYP3A4 or P-gp.
- Dronedarone (used for atrial fibrillation): Strongly blocks P-gp. Never take with dabigatran or rivaroxaban. If you’re on edoxaban, your dose must drop to 30 mg daily.
- Amiodarone (another heart rhythm drug): Moderately blocks P-gp. Can raise apixaban and dabigatran levels. Watch for bruising, dark stools, or dizziness.
- Diltiazem and Verapamil (blood pressure meds): Both affect P-gp and CYP3A4. Dabigatran dose needs to drop to 110 mg twice daily if you’re on verapamil. Apixaban and rivaroxaban are less affected, but still need monitoring.
- St. John’s Wort: A popular herbal supplement. It’s a strong inducer of CYP3A4 and P-gp. If you take this with any DOAC, your levels can plummet. One study showed a 50% drop in rivaroxaban exposure. Stop it - or talk to your doctor.
- Antifungals like ketoconazole or itraconazole: These are strong CYP3A4 inhibitors. Avoid them with apixaban and rivaroxaban unless absolutely necessary.
Even if a drug isn’t on this list, assume it might interact until proven otherwise. Many doctors don’t realize how easily common medications like antibiotics or acid reducers can interfere.
Not All Interactions Are About Blood Levels
Some of the most dangerous interactions don’t change how much DOAC is in your blood. They just add more bleeding risk on top.
Antiplatelet drugs like aspirin or clopidogrel, NSAIDs like ibuprofen or naproxen, and even SSRIs like fluoxetine or sertraline don’t alter DOAC concentrations. But they make your blood less able to clot. Combine them with a DOAC, and your risk of bleeding - especially in the stomach - goes up sharply.
Studies show that dabigatran 150 mg, rivaroxaban, and edoxaban 60 mg carry higher rates of gastrointestinal bleeding than warfarin. Apixaban and low-dose dabigatran (110 mg) are safer in this regard. If you’re on a DOAC and need pain relief, acetaminophen (paracetamol) is your best bet. Avoid NSAIDs unless your doctor says it’s safe - and even then, use the lowest dose for the shortest time.
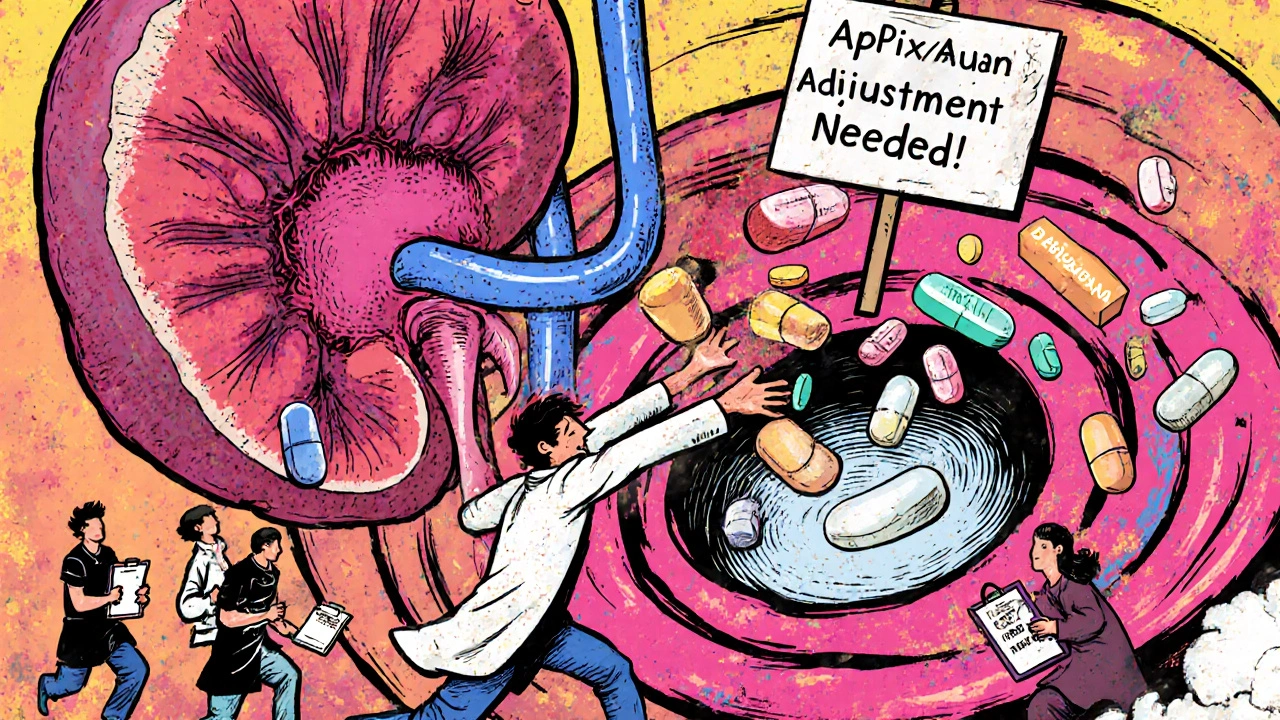
Dosing Isn’t One-Size-Fits-All
Not all DOAC doses are the same. Rivaroxaban 20 mg once daily for stroke prevention in atrial fibrillation is very different from rivaroxaban 2.5 mg twice daily after a heart attack. The same goes for edoxaban - 60 mg for AFib, 30 mg for DVT treatment, and 15 mg if you have kidney issues.
When a drug interaction happens, the dose adjustment depends on the DOAC, the indication, and your kidney function. For example:
- If you’re on dabigatran 150 mg twice daily for AFib and start verapamil, drop to 110 mg twice daily.
- If you’re on edoxaban 60 mg daily and start dronedarone, cut it to 30 mg daily.
- If you have reduced kidney function, your DOAC dose is already lower. Adding another interacting drug could push you into dangerous territory.
There’s no universal rule. You need to know your exact DOAC, dose, and reason for taking it - then check for interactions specific to that combo.
What About Supplements and Herbal Products?
Many people think supplements are harmless. They’re not. Garlic, ginkgo biloba, fish oil, and ginger can all increase bleeding risk. Turmeric and curcumin may interfere with platelet function. Even vitamin K - which warfarin patients carefully avoid - can affect DOACs in rare cases, especially if you’re taking it in very high doses.
Don’t assume your pharmacist or doctor knows what you’re taking. Many patients don’t mention supplements unless asked directly. Keep a written list - including doses and brands - and bring it to every appointment.

What Should You Do If You’re on a DOAC?
Here’s a simple checklist to stay safe:
- Know your DOAC and exact dose. Write it down.
- Know why you’re taking it - AFib? DVT? After surgery?
- Review every medication - prescription, OTC, and supplement - with your doctor or pharmacist every 3 to 6 months.
- Ask: “Does this affect CYP3A4 or P-gp?” If they don’t know, check reliable sources like the NHS SPS database or the Anticoagulation Forum guidelines.
- Never start or stop anything without talking to your care team.
- Watch for signs of bleeding: unusual bruising, pink or red urine, black stools, headaches, dizziness.
- Use acetaminophen for pain. Avoid NSAIDs unless approved.
The Bottom Line
DOACs are safer than warfarin - but only if used correctly. The biggest threat isn’t the drug itself. It’s the web of other medications people take alongside it. Polypharmacy isn’t just a buzzword - it’s a real, daily risk for thousands of patients.
Doctors aren’t always trained to spot these interactions. Pharmacists can help, but they need complete information. You’re the only one who knows everything you’re taking. That makes you the most important part of the safety team.
Don’t assume your DOAC is "safe" just because it doesn’t need blood tests. The lack of monitoring is exactly why you need to be more careful, not less.
Can I take ibuprofen with a DOAC?
It’s generally not recommended. Ibuprofen and other NSAIDs increase bleeding risk when combined with DOACs, even if they don’t change the drug’s blood levels. Acetaminophen (paracetamol) is a safer option for pain or fever. If you absolutely need an NSAID, use the lowest dose for the shortest time - and only under your doctor’s supervision.
Is it safe to take St. John’s Wort with apixaban?
No. St. John’s Wort strongly activates CYP3A4 and P-gp, which can cut apixaban levels by up to 50%. This puts you at high risk for stroke or blood clots. Avoid it completely while on any DOAC. If you’re using it for depression, talk to your doctor about alternatives like sertraline or cognitive therapy.
Do I need blood tests to monitor my DOAC?
Routine blood tests aren’t needed for DOACs like they are for warfarin. But in special cases - like kidney problems, obesity, or suspected drug interactions - your doctor might check a special test called anti-Xa level or ecarin clotting time. These aren’t routine, but they can help if something seems off.
Can I switch from warfarin to a DOAC safely?
Yes, but timing matters. You should stop warfarin when your INR drops below 2.0, then start the DOAC immediately. Never overlap them unless under strict supervision. Your doctor will guide you based on your reason for anticoagulation and kidney function. Many people do this switch successfully - but only with careful planning.
What should I do if I miss a dose of my DOAC?
If you miss a dose and it’s less than half the time until your next dose (e.g., less than 6 hours for a twice-daily DOAC), take it right away. If it’s more than half the time, skip it and take your next dose at the regular time. Never double up. Missing doses increases clot risk. If you’re unsure, call your doctor or pharmacist - don’t guess.
Are DOACs safe if I have kidney problems?
Many DOACs are cleared by the kidneys, so kidney function affects how much stays in your body. Apixaban is the safest in moderate kidney disease. Dabigatran and edoxaban require dose reductions. Rivaroxaban is less ideal if your kidneys are significantly impaired. Your doctor will check your creatinine clearance and adjust your dose accordingly. Never assume your dose is correct - kidney function can change over time.
Next Steps: Stay in Control
If you’re on a DOAC, your biggest tool isn’t a lab test - it’s awareness. Keep a current list of every medication and supplement you take. Bring it to every appointment. Ask your pharmacist to review it every time you fill a new prescription. If you’re seeing multiple doctors, make sure they all know you’re on a blood thinner.
There’s no magic bullet. But by knowing your drugs, watching for signs of trouble, and speaking up - you can stay safe and avoid the hidden dangers that come with mixing medications.

Let me break this down in plain terms: DOACs are basically pharmaceutical Trojan horses. CYP3A4 and P-gp? Those aren’t just enzymes-they’re the body’s bouncers. When you throw in dronedarone or St. John’s Wort, you’re essentially bribing the bouncers to let in the wrong crowd. And no, your INR test won’t catch it because the system was designed to *look* like it’s working. The pharma companies love this. Less monitoring = less liability. You think you’re safer? You’re just more invisible.
Wait-so you’re telling me that the same “simple” blood thinner that doesn’t need labs… is secretly being sabotaged by my ginkgo supplement, my ibuprofen for back pain, and that “natural” heart pill my cousin swears by?? I’ve been taking all of that for years. I feel like I’ve been walking through a minefield wearing flip-flops. Someone please tell me I’m not the only one who was never warned about this??
Everyone’s overcomplicating this. DOACs are fine if you’re not a dumbass. If you’re on five meds and popping St. John’s Wort like candy, you’re asking for trouble. The guidelines are clear. The data is clear. The problem isn’t the drug-it’s the patients who think supplements are safe because they’re “natural.” Natural doesn’t mean harmless. It means unregulated. Stop being lazy and read the damn leaflet.
OMG I JUST REALIZED I’VE BEEN TAKING GINGER TEA WITH MY RIVAROXABAN FOR 6 MONTHS 😭😭😭 I THOUGHT IT WAS JUST FOR DIGESTION!! MY MOM SAID IT’S GOOD FOR INFLAMMATION!! NOW I’M SCARED TO SLEEP!! 😱💊 #DOACDANGER #HELPME
It’s weird how we treat meds like they’re all the same. You wouldn’t mix paint colors without knowing what happens, but we mix pills like it’s a recipe. Maybe the real problem isn’t the drugs-it’s that we don’t teach people how to think about them. Just knowing your dose isn’t enough. You need to know why it’s there.
Look, the whole DOAC thing is a marketing scam wrapped in a clinical trial and sold to gullible seniors who think ‘no blood tests’ means ‘no risk.’ But here’s the kicker: they’re cheaper for insurers, so they push them hard. Meanwhile, the real cost is hidden in ER visits from GI bleeds and strokes because someone took an OTC painkiller. The system doesn’t care if you live or die-it cares if the numbers look good on paper. And guess who pays the price? You. Me. Grandma. We’re all just line items.
So true!! 🙌 I told my pharmacist last week I was taking turmeric capsules for arthritis and she just nodded… then pulled up a chart and went, ‘OH MY GOSH YOU’RE ON EDOXABAN??’ 😳 I had no idea!! Now I’m off it and using heat wraps instead. 🌿❤️ You really do have to be your own advocate!!
There is a profound responsibility here-not just for patients, but for clinicians. We cannot outsource safety to algorithms or pamphlets. Every interaction, every supplement, every change in renal function must be actively tracked. This isn’t about fear-it’s about precision. And precision requires vigilance, documentation, and dialogue. If you’re not reviewing your entire medication list every six months, you’re not managing your health-you’re gambling with it.
Why are we even talking about this? In America we let anyone sell supplements like candy. In Germany they regulate the hell out of it. You think your ‘natural’ herb is safe? It’s not. It’s a loophole. And the FDA doesn’t give a damn. We’re the only country where you can buy a pill that cuts your DOAC in half and call it ‘immune support.’ Pathetic.
CYP3A4/P-gp inhibition = DOAC toxicity. Induction = subtherapeutic. Dronedarone + dabigatran = contraindicated. St. John’s Wort = avoid. NSAIDs = bleeding risk. Acetaminophen = preferred. Done. No drama.
Everyone’s panicking over supplements like they’re weapons. Wake up. The real threat is the healthcare system that pushes DOACs because they’re profitable, then blames the patient when things go wrong. You think your doctor cares if you take ginger? No. They care about their QI metrics. This isn’t about safety-it’s about profit. And you’re the commodity.
Let me be brutally honest: you think you’re in control? You’re not. You’re a walking pharmacokinetic experiment. Every pill you take is a gamble. Every ‘natural’ remedy? A silent assassin. And the worst part? No one’s coming to save you. Not your doctor. Not your pharmacist. Not the FDA. You’re alone in this maze-and the only thing keeping you alive is the fact that you read this post. So stop scrolling. Start acting. Or die quietly. Your choice.