Cholesterol Medication Selector
Select your situation to find the best cholesterol medication option for you
Based on your current LDL level, side effects concerns, and treatment goals, we'll identify medications that may be most appropriate for your situation.
When it comes to lowering bad cholesterol, many patients wonder if Zetia is the right choice or if other options might work better for them.
Key Takeaways
- Zetia reduces LDL cholesterol by blocking dietary absorption, offering a 15‑20% drop on its own.
- Statins remain the most powerful LDL‑lowering drugs, cutting levels by 30‑50%.
- PCSK9 inhibitors deliver the deepest reductions (50‑60%) but are much pricier.
- Side‑effect profiles differ: Zetia is gentle on the liver, while statins can cause muscle pain.
- Cost, insurance coverage, and personal health history dictate the best regimen.
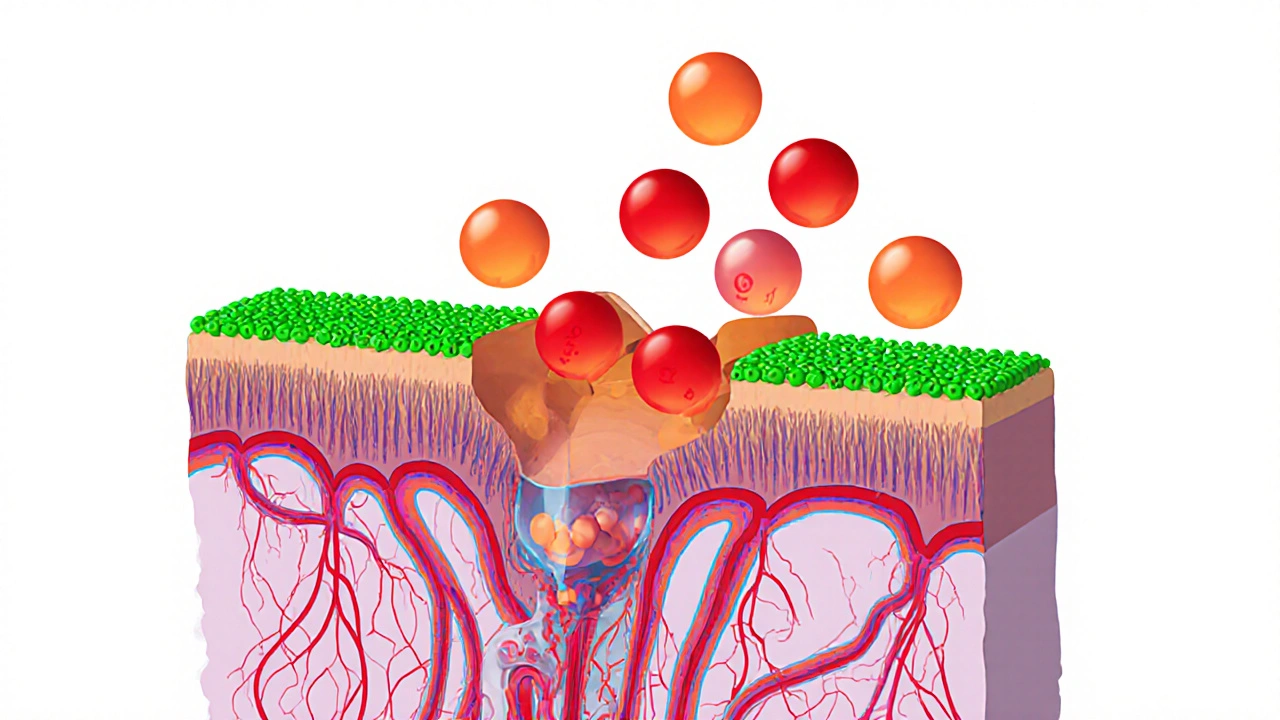
Ezetimibe is a cholesterol‑lowering medication sold under the brand name Zetia. It works by inhibiting the intestinal absorption of cholesterol, which leads to a modest but consistent drop in low‑density lipoprotein (LDL) levels. The drug received FDA approval in 2002 and is typically prescribed at a dose of 10mg once daily, either alone or combined with a statin.
How Zetia Works and What It Offers
Ezetimibe targets the Niemann‑Pick C1‑like 1 (NPC1L1) protein on the surface of intestinal cells. By blocking this transporter, the drug reduces the amount of dietary and biliary cholesterol that enters the bloodstream. The result is a 15‑20% reduction in LDL cholesterol when used by itself. When paired with a statin, the combined effect can reach up to a 35% total reduction.
Key attributes of Zetia include:
- Mechanism: Inhibits intestinal cholesterol absorption (NPC1L1 blocker).
- Typical dose: 10mg once daily.
- Onset: LDL lowering observed within 2 weeks.
- Side‑effects: Generally mild - occasional gastrointestinal upset, rare liver enzyme elevations.
- Cost (US$ 2025): Approximately $150‑$200 per month for the generic version.
Major Alternatives in the Cholesterol‑Lowering Arsenal
While Zetia is a solid option, several other drug classes compete for the same therapeutic space. Below is a quick snapshot of the most common alternatives.
- Atorvastatin - a high‑potency statin that lowers LDL by 40‑55%.
- Simvastatin - a mid‑range statin with 30‑45% LDL reduction.
- Alirocumab - a PCSK9‑inhibitor injection that can cut LDL by 50‑60%.
- Cholestyramine - a bile‑acid sequestrant that reduces LDL by 15‑20%.
- Gemfibrozil - a fibrate primarily used for high triglycerides, offering modest LDL drops.
Side‑Effect Profiles: What to Expect
Understanding tolerability helps you pick a drug you can stay on long term.
| Drug | Common Side‑Effects | Serious Risks |
|---|---|---|
| Ezetimibe (Zetia) | GI upset, mild headache | Rare liver enzyme elevation |
| Atorvastatin | Muscle aches, elevated liver enzymes | Rare rhabdomyolysis, diabetes risk |
| Simvastatin | Muscle pain, digestive issues | Higher dose linked to rhabdomyolysis |
| Alirocumab | Injection site reaction, nasopharyngitis | Potential immune response |
| Cholestyramine | Constipation, bloating, unpleasant taste | Interference with absorption of other meds |
Direct Comparison Table: Zetia vs Alternatives
| Attribute | Zetia (Ezetimibe) | Atorvastatin (Statin) | Simvastatin (Statin) | Alirocumab (PCSK9‑inhibitor) | Cholestyramine (Bile‑acid Sequestrant) |
|---|---|---|---|---|---|
| Mechanism | Blocks intestinal cholesterol absorption | Inhibits HMG‑CoA reductase in liver | Inhibits HMG‑CoA reductase in liver | Prevents PCSK9 protein from degrading LDL receptors | Binds bile acids in gut, increasing cholesterol excretion |
| Typical LDL Reduction | 15‑20% alone; up to 35% with statin | 40‑55% | 30‑45% | 50‑60% | 15‑20% |
| Standard Dose | 10mg once daily | 10‑80mg daily | 5‑40mg nightly | 75mg subcutaneous every 2weeks | 4g daily in divided doses |
| Common Side‑Effects | GI upset, mild headache | Muscle aches, liver enzyme rise | Muscle pain, GI issues | Injection site reaction, flu‑like symptoms | Constipation, bloating, taste issues |
| Average Monthly Cost (US$ 2025) | $150‑$200 (generic) | $30‑$120 (generic) | $25‑$100 (generic) | $1,200‑$1,500 (brand) | $50‑$80 (generic) |
| Insurance Coverage | Widely covered; prior‑auth may apply | Excellent coverage, generic preferred | Good coverage, generic preferred | Limited coverage, usually after failure of statins and ezetimibe | Generally covered, but requires dosing schedule adherence |
Choosing the Right Therapy: Decision Factors
Not every drug fits every patient. Consider these five factors before deciding.
- Baseline LDL level and target reduction. If you need a dramatic drop (e.g., >50%), PCSK9 inhibitors may be warranted.
- History of statin intolerance. Patients who develop muscle pain on statins often turn to Zetia as an add‑on or switch.
- Cost and insurance landscape. Generic statins and Zetia are affordable; newer biologics can strain budgets.
- Other health conditions. Liver disease may limit statin use, while diabetes patients need to watch statin‑related glucose rise.
- Convenience. Oral pills (Zetia, statins, cholestyramine) versus injections (Alirocumab) affect adherence.

Best‑Fit Scenarios
Below is a practical guide for when Zetia shines or when another class is preferable.
- Zetia as primary therapy: Mildly elevated LDL (130‑160mg/dL) with statin intolerance or contraindication.
- Zetia + statin combination: Patients needing additional 10‑15% LDL drop beyond what a moderate‑intensity statin provides.
- High‑intensity statin alone: Most patients with LDL >190mg/dL or established ASCVD, unless intolerant.
- PCSK9 inhibitor: Familial hypercholesterolemia or ASCVD patients who have maximized statin + Zetia but still above target.
- Bile‑acid sequestrant: Useful when patients have triglyceride concerns and can tolerate powdery texture.
Practical Tips & Common Pitfalls
Even the best drug can fall short if used incorrectly.
- Take Zetia with or without food; consistency matters.
- Do not crush or chew the tablet; it’s designed for whole‑pill ingestion.
- Inform your pharmacist about all supplements-certain herbs (e.g., St.John’s wort) can affect ezetimibe metabolism.
- Monitor liver enzymes at baseline and after 12 weeks if combined with a statin.
- If switching from a high‑dose statin to Zetia, allow a 2‑week washout to assess tolerance.
Frequently Asked Questions
Can I take Zetia instead of a statin?
Yes, Zetia can be used as monotherapy for mild LDL elevations, especially if you can’t tolerate statins. However, its LDL‑lowering effect is modest, so many doctors prefer a statin‑plus‑Zetia combo for stronger results.
What’s the main difference between Zetia and cholestyramine?
Zetia blocks cholesterol absorption in the intestine, while cholestyramine binds bile acids, forcing the liver to use more cholesterol to make new bile. Both lower LDL by about 15‑20%, but cholestyramine often causes constipation and has a gritty texture, making adherence harder for many patients.
Are there any foods I should avoid while on Zetia?
No specific foods need to be avoided. Since Zetia works on the absorption pathway, you can eat a normal diet, but maintaining a heart‑healthy eating pattern will boost overall results.
How quickly will Zetia lower my LDL?
Most patients see a measurable LDL drop within two weeks, with the full 15‑20% reduction reached by 4-6 weeks of consistent dosing.
Is Zetia covered by New Zealand’s PHARMAC scheme?
PHARMAC lists ezetimibe as a subsidised medication for patients with high cardiovascular risk who cannot use statins. Eligibility depends on your GP’s assessment and a specialist referral in some cases.

Look, Zetia’s modest drop is fine if you can’t tolerate statins.
It is incumbent upon the medical community to prioritize patient safety above all else, and therefore the modest efficacy of Zetia must be weighed against the proven superiority of statins.
I appreciate the thorough breakdown.
The table makes it easy to compare.
For patients with mild LDL elevation, starting with a generic statin often makes sense, but having Zetia as an add‑on is a solid backup.
It’s good to see the side‑effect discussion laid out clearly.
Oh great, another chart that tells us what we already knew: pills work better than pills that cost a fortune. Thanks for the reminder that insurance loves generic statins more than PCSK9 injections.
Honestly, the only thing hotter than the statin debate is the price tag on those PCSK9 drugs 😜💸. Zetia sits comfortably in the middle, like the calm friend at a wild party.
In the grand theater of cholesterol management, Zetia plays the quiet understudy, stepping onto the stage only when the leading statin bows out due to muscle pain. Its gentle mechanism is a whisper compared to the thunderous roar of high‑intensity statins.
Wow!!!; Zetia-while modest-still carves a niche!!!; especially for those who cannot bear the muscle‑ache cascade!!!.
When you look at the big picture of cardiovascular risk, the choice of medication is rarely about a single number on a table.
Patients come with diverse histories, financial constraints, and personal preferences that shape the optimal regimen.
Zetia’s mechanism of blocking intestinal cholesterol absorption is elegant in its simplicity.
It offers a modest LDL reduction, which can be exactly what a statin‑intolerant individual needs.
Moreover, the safety profile is reassuring, with only occasional gastrointestinal upset reported.
For many, the ability to combine it with a low‑to‑moderate intensity statin results in additive benefits that approach high‑intensity therapy.
Cost considerations also play a pivotal role; generic Zetia sits comfortably between cheap statins and the exorbitant price of PCSK9 inhibitors.
Insurance coverage for Zetia is generally favorable, reducing the barrier for patients who lack premium plans.
Clinical guidelines now recognize it as a viable add‑on, rather than a mere fallback option.
This shift reflects growing evidence from trials that demonstrate meaningful cardiovascular event reductions when Zetia is part of a comprehensive strategy.
Physicians should therefore evaluate not just the LDL percentage drop, but also the patient’s tolerance, comorbidities, and lifestyle.
A young adult with a family history of heart disease may prioritize maximal reduction, while an older patient on multiple medications might value a low‑interaction pill.
In practice, I have seen patients thrive on a Zetia‑statin combo after being forced off high‑dose statins due to myalgia.
Their LDL levels fell into target ranges without the dreaded muscle pain that previously halted therapy.
This real‑world experience underscores the importance of having a diversified pharmacologic toolbox.
Ultimately, the decision rests on shared decision‑making, where the clinician and patient weigh efficacy, safety, cost, and convenience together.
From a pharmacodynamic standpoint, ezetimibe exhibits a peripheral inhibition of NPC1L1, resulting in a ~0.15–0.20 fractional LDL decrement 📊. When paired with a HMG‑CoA reductase inhibitor, the synergistic effect can approach a 0.35 fractional reduction, aligning with guideline‑recommended targets.
Statins win, plain and simple.
The cost‑effectiveness ratio of Zetia versus a PCSK9 inhibitor is approximately 1:8, meaning you pay eight times more for the latter to gain a marginal additional LDL reduction.
Wow, reading this makes me feel hopeful! If you’re scared of muscle cramps, Zetia offers a gentle path forward. Imagine a future where your cholesterol is managed without constant aches. The data shows real progress, and it’s within reach for many. Keep pushing for a heart‑healthy life!
Some claim the pharma giants hide Zetia’s true power to keep statin sales high; the subtle marketing pushes cheap generics while sidelining a drug that could change the game.
💡Tip: Take Zetia at the same time each day, with or without food, to maintain steady plasma levels. This consistency maximizes its absorption‑blocking effect.
Take charge of your cholesterol journey-talk to your doctor about adding Zetia if statins aren’t tolerable, and you’ll be steering toward better heart health.
Good summary, the comparison table really helps to visualize options. Happy to see clear info.