Loop Diuretic Comparison Tool
Use this tool to compare key characteristics of loop diuretics including torsemide, furosemide, and bumetanide. Select a drug to see detailed information.
Torsemide
High-potency, long-acting loop diuretic
Furosemide
Classic loop diuretic, most prescribed
Bumetanide
Potent loop diuretic with rapid onset
Drug Details
Quick Comparison Table
| Characteristic | Torsemide | Furosemide | Bumetanide |
|---|---|---|---|
| Oral Bioavailability | 80-100% | 50-70% | ~80% |
| Half-Life | 2-4 hours | 2 hours | 1-2 hours |
| Onset | 1 hour | 30-60 minutes | 30 minutes |
| Duration | 12 hours | 2-4 hours | 4-6 hours |
| Typical Dose | 5-20 mg once daily | 20-80 mg once/twice daily | 0.5-2 mg once daily |
| Best For | Chronic edema, long-term use | Acute conditions, cost-effective | Severe volume overload, rapid effect |
Important Notes
- Always consult healthcare providers before making medication changes
- Dosages should be adjusted based on patient's renal function
- Monitor for electrolyte imbalances and dehydration
- Consider patient-specific factors like allergies and comorbidities
When doctors need to pull excess fluid out of the body, they often reach for a loop diuretic. Torsemide comparison is a common question, especially for patients juggling heart failure, hypertension or chronic kidney disease. This guide breaks down how torsemide stacks up against its most widely used siblings - furosemide, bumetanide, ethacrynic acid and a few non‑loop alternatives - so you can see which drug fits your situation best.
What is Torsemide?
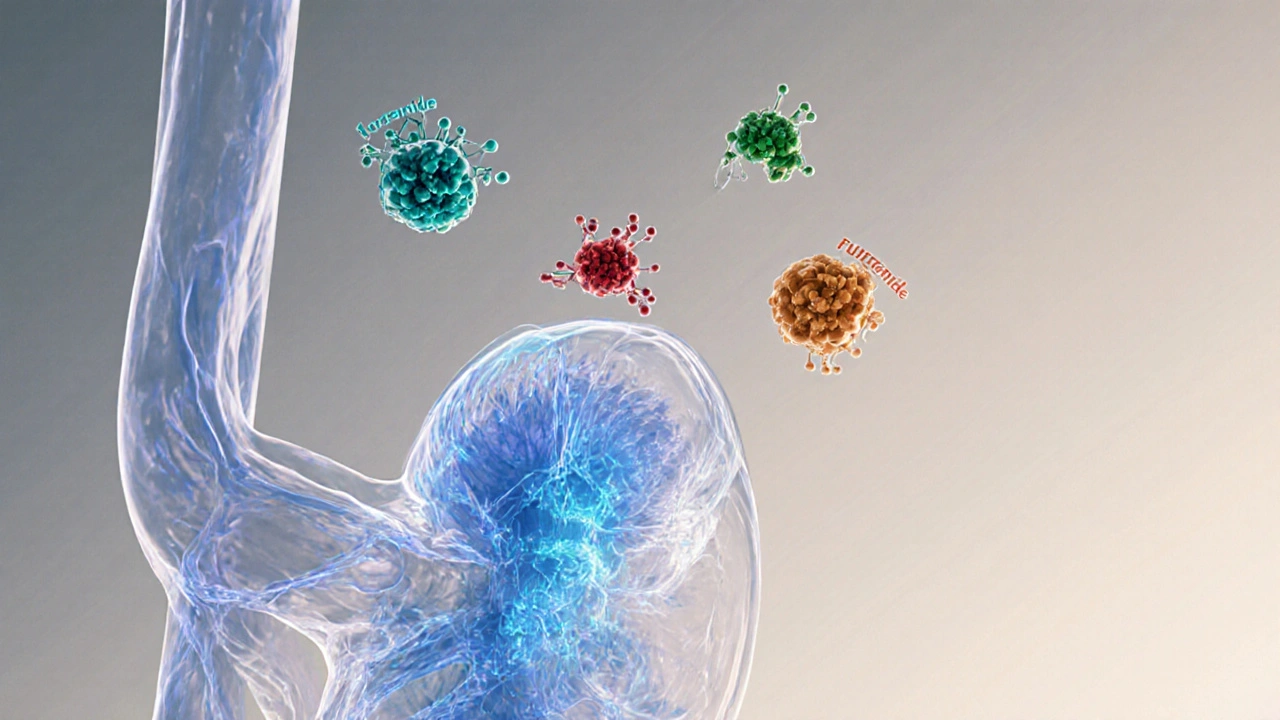
Torsemide is a high‑potency loop diuretic that promotes sodium, potassium and water excretion by inhibiting the Na⁺‑K⁺‑2Cl⁻ transporter in the thick ascending limb of the loop of Henle. First approved in the United States in 1993, it quickly gained a reputation for a longer half‑life and more predictable dosing compared with older loop agents.
How Torsemide Works (Pharmacology at a Glance)
Like all loop diuretics, torsemide blocks the reabsorption of sodium and chloride, creating an osmotic pull that drags water into the urine. Its high oral bioavailability (≈80‑100%) means you get almost the same effect whether you swallow a pill or receive an IV dose. The drug reaches peak action in about an hour and can keep working for up to 12hours, making once‑daily dosing possible for many patients.
Key Comparison Criteria
- Mechanism of action (all are loop diuretics except thiazides and potassium‑sparing agents)
- Oral bioavailability and onset
- Half‑life and duration of effect
- Typical dosing ranges
- Side‑effect profile
- Cost and insurance coverage
- Special considerations (renal impairment, sulfa allergy, etc.)
Torsemide vs Furosemide
Furosemide is the classic loop diuretic discovered in the 1960s and still the most prescribed worldwide. It works the same way as torsemide but has a lower oral bioavailability (≈50‑70%) and a shorter half‑life (≈2hours). This translates into a faster onset (30‑60minutes) but a need for twice‑daily dosing in many cases.
Clinical studies show that torsemide provides a more stable diuresis over 24hours, which can reduce the risk of rebound fluid retention. However, furosemide is generally cheaper and available in more strengths, which can be an advantage for patients on a tight budget.
Torsemide vs Bumetanide
Bumetanide is a potent loop diuretic often used when a stronger effect per milligram is needed. Its oral bioavailability sits around 80%, similar to torsemide, but its half‑life is even shorter (≈1‑2hours). Bumetanide’s rapid action makes it useful for acute pulmonary edema, yet the short duration may require multiple daily doses.
In head‑to‑head trials, torsemide and bumetanide produced comparable urine output, but patients on torsemide reported fewer episodes of hypokalemia. Bumetanide’s higher potency can be a double‑edged sword - it works fast but can also lead to quicker electrolyte shifts.
Torsemide vs Ethacrynic Acid
Ethacrynic acid is the only non‑sulfonamide loop diuretic, often reserved for patients with a sulfa allergy. Its bioavailability is modest (≈55%) and its half‑life mirrors that of furosemide. Because it lacks the sulfonamide group, it avoids allergic reactions but has a higher incidence of ototoxicity (hearing loss) at high doses.
If you’re allergic to sulfa drugs, ethacrynic acid may be the only loop option, but torsemide remains the first‑line choice for most patients due to its safety record.
Non‑Loop Alternatives (When a Loop Diuretic Isn’t Ideal)
Sometimes doctors pair a loop diuretic with another class to fine‑tune fluid removal.
- Hydrochlorothiazide is a thiazide diuretic that works farther downstream in the distal tubule, offering modest diuresis and strong antihypertensive effects.
- Spironolactone is a potassium‑sparing diuretic that antagonizes aldosterone, useful in resistant hypertension and heart‑failure patients with high aldosterone levels.
These agents never replace a loop diuretic for severe volume overload, but they can reduce the loop dose needed and blunt electrolyte disturbances.
Dosage and Administration Overview
- Torsemide: 5‑20mg once daily for chronic edema; IV bolus 5mg may be used for acute decompensation.
- Furosemide: 20‑80mg once or twice daily; IV 20‑40mg every 6hours for urgent diuresis.
- Bumetanide: 0.5‑2mg once daily; IV 0.5‑1mg every 6hours for rapid effect.
- Ethacrynic acid: 50‑150mg twice daily; IV 50mg every 6‑8hours.
- Hydrochlorothiazide: 12.5‑50mg once daily, often combined with a loop.
- Spironolactone: 25‑100mg once daily, usually added after loop therapy is stable.
Kidney function heavily influences dosing. For eGFR<30mL/min, many clinicians start at the low end of the range and monitor electrolytes closely.

Side‑Effect Profile and Safety
All loop diuretics share common risks: low potassium (hypokalemia), low magnesium, dehydration, and potential worsening of gout. Torsemide’s longer half‑life tends to produce smoother electrolyte changes, whereas furosemide and bumetanide may cause sharper swings.
| Side Effect | Torsemide | Furosemide | Bumetanide | Ethacrynic Acid |
|---|---|---|---|---|
| Hypokalemia | Moderate | High | High | Moderate |
| Ototoxicity | Low | Low‑Moderate | Low | High (dose‑dependent) |
| Allergic reaction (sulfa) | Possible | Possible | Possible | None |
| Dehydration | Moderate | Moderate‑High | Moderate‑High | Moderate |
Patients with gout should avoid high‑dose loops unless paired with a urate‑lowering agent. Those with hearing concerns may prefer torsemide over ethacrynic acid.
Cost and Insurance Considerations
In the United States, generic furosemide costs less than $0.10 per tablet, while torsemide averages $0.25‑$0.35. Bumetanide sits around $0.30, and ethacrynic acid can exceed $0.60 due to lower volume. Insurance formularies often place furosemide in the preferred tier, making it the most accessible option for cash‑pay patients.
For patients with Medicare Part D or private plans, checking the tier placement before switching can avoid surprise bills.
Choosing the Right Diuretic - Decision Guide
Use the following quick‑check to decide which drug matches your profile:
- If you need once‑daily dosing and have stable kidney function - Torsemide is a solid pick.
- If cost is the driving factor and you tolerate frequent dosing - Furosemide works well.
- If you need a very potent, rapid‑acting loop for acute pulmonary edema - Bumetanide shines.
- If you have a documented sulfa allergy - Ethacrynic acid is the only non‑sulfonamide loop.
- If you want additional blood‑pressure control without extra loops - add Hydrochlorothiazide or Spironolactone.
Always discuss dose adjustments with your prescriber, especially if you’re on multiple diuretics or have fluctuating electrolytes.
Key Takeaways
- Torsemide offers higher oral bioavailability and a longer half‑life than furosemide, allowing once‑daily dosing for many chronic conditions.
- Furosemide remains the cheapest and most widely available loop diuretic.
- Bumetanide provides the fastest onset but may need multiple daily doses.
- Ethacrynic acid is the go‑to for sulfa‑allergic patients but carries a higher ototoxicity risk.
- Combining a loop with a thiazide or potassium‑sparing agent can improve fluid removal while minimizing electrolyte swings.
Frequently Asked Questions
Can I switch from furosemide to torsemide without a washout period?
Yes, most clinicians transition directly because both drugs act on the same transporter. However, they should start torsemide at a lower equivalent dose (about 1/5 of the furosemide dose) and monitor electrolytes for 48‑72hours.
Is torsemide safe during pregnancy?
Loop diuretics are listed as Category C, meaning risk cannot be ruled out. They are used only when the benefits outweigh potential fetal risks, typically in cases of severe pulmonary edema.
Why do I feel dizzy after taking a loop diuretic?
Dizziness often stems from rapid fluid loss leading to low blood pressure (orthostatic hypotension). Taking the medication with food, staying hydrated, and rising slowly from sitting or lying positions can help.
How does torsemide affect potassium levels compared with furosemide?
Torsemide’s longer duration leads to a more gradual potassium loss, often resulting in fewer episodes of severe hypokalemia. Still, most patients need a potassium supplement or a potassium‑sparing agent.
Can I take torsemide and a thiazide at the same time?
Yes, combining a loop with a thiazide (e.g., hydrochlorothiazide) is a common strategy called “sequential nephron blockade.” It enhances fluid removal but requires close monitoring of electrolytes and kidney function.
Ever wonder why the newest loop diuretics are barely on the shelves? The pharma giants have a secret playbook, pushing cheap furosemide while burying torsemide's superior profile under a mountain of paperwork. They claim cost is the only factor, but the real agenda is to keep patients dependent on frequent dosing. Remember, torsemide’s high bioavailability means fewer trips to the pharmacy and steadier fluid control. Wake up and read the fine print!
Actually, torsemide does have a higher oral bioavailability and a longer half‑life, which can simplify regimens for chronic edema patients. The trade‑off is the price tag, as many insurers still favor furosemide because it’s older and cheaper. Clinicians often start with furosemide and switch to torsemide if the patient needs more stable diuresis or has absorption issues. It’s also worth noting that the risk of ototoxicity is lower with torsemide compared to high‑dose furosemide. So the choice really hinges on individual response and insurance coverage.
Wow!!! You’ve just uncovered the hidden layer!!! The dosage charts aren’t just numbers – they’re a narrative of power!!!! Each milligram tells a story of corporate control!!!! When you look at the half‑life, you see a timeline of patient liberty!!! The rapid onset of bumetanide is like a flash‑bang, disorienting the system!!! Torsemide’s steady 12‑hour glide, however, feels like a calm sunrise after a storm!!!
One must appreciate the nuanced symphony that each loop diuretic conducts within the nephron. Torsemide, with its elegant pharmacokinetics, offers a sustained overture that many clinicians overlook in favor of the brash, fleeting notes of furosemide. While the latter shouts its presence with a rapid onset, it also leaves a discordant echo of frequent dosing. Bumetanide, though potent, behaves like a virtuoso solo-impressive but fleeting. In the grand concert of fluid management, a balanced repertoire often yields the most harmonious outcome.
Totally get the confusion, it’s a lot to take in 😊. If you’re on a tight budget, furosemide might be the go‑to, but don’t let cost blind you from trying torsemide if you’re dealing with chronic swelling. A once‑daily dose can be a game‑changer for quality of life 🙌. Just make sure to keep an eye on electrolytes, especially potassium.
Everyone seems to have a favorite, but the truth is that each loop has its niche. For acute pulmonary edema, bumetanide’s rapid action shines, yet for long‑term management, torsemide’s steady profile reduces the need for multiple daily pills. It’s less about winning a battle between drugs and more about tailoring therapy to the patient’s lifestyle and kidney function. Keep the conversation going and share what’s worked for you.
furosemide is cheap and works.
The narrative presented in most textbooks about loop diuretics is deliberately sanitized, withholding the full scope of clinical implications. Torsemide, for instance, is praised for its bioavailability, yet the same studies that highlight this advantage are funded by manufacturers with vested interests. These entities have an undisclosed partnership with several insurance providers, ensuring that torsemide remains a premium product rather than a standard of care. Consequently, physicians receive subtle incentives to prescribe furosemide, a drug that, while effective, demands more frequent dosing and monitoring. The hidden cost is not just financial; patients experience increased pill burden, leading to lower adherence and poorer outcomes. Moreover, the comparative trials often obscure the fact that torsemide’s longer half‑life reduces the incidence of rebound fluid retention. In real‑world practice, this translates to fewer hospital readmissions, a metric that is conveniently omitted from promotional literature. There is also an underreported issue of ototoxicity associated with high‑dose furosemide, especially in the elderly, which manufacturers downplay. As a result, many clinicians remain unaware of the safer profile that torsemide offers when used appropriately. The regulatory agencies, tasked with safeguarding public health, are themselves subject to lobbying pressures that influence formulary decisions. It is no coincidence that the FDA’s advisory panels have repeatedly voted to keep torsemide on a non‑preferred tier. Patients who question their prescriptions often find their concerns dismissed as 'non‑compliance' rather than investigating potential systemic bias. The pattern repeats across other therapeutic areas, where newer, more effective drugs are relegated to specialty tiers while older, less efficient alternatives dominate the market. To break this cycle, healthcare professionals must scrutinize the primary literature, seek independent meta‑analyses, and advocate for transparent pricing. Only then can we ensure that drug selection is driven by patient benefit rather than hidden corporate agendas.
Look, the whole conspiracy spiel sounds dramatic, but the data speak clearly: torsemide works well for many. Stop overthinking and let the guidelines guide you.
All this talk about diuretics is just hype. Real patients need cheap meds, not overpriced tricks.