Statins & Diabetes Risk Calculator
Personal Risk Assessment
Many people take statins to lower cholesterol and protect their heart. But if you’ve noticed your blood sugar creeping up after starting a statin, you’re not alone. Research shows that for some people, these heart-protecting drugs can nudge blood sugar levels higher - enough to push someone with prediabetes into full-blown type 2 diabetes. It’s not common for everyone, but it’s real, measurable, and worth understanding before you start or continue taking statins.
How Statins Affect Blood Sugar
Statins don’t cause diabetes out of nowhere. Instead, they make it easier for people who are already at risk to cross the line. The main way this happens is by interfering with how your body uses insulin. Two key things go wrong: your muscles and liver become less sensitive to insulin (insulin resistance), and your pancreas doesn’t release as much insulin as it should (reduced insulin secretion).
A large study of nearly 9,000 people in Finland tracked those on statins over six years. The results showed a 46% higher chance of developing type 2 diabetes compared to those not taking statins. That’s not a huge number for any single person, but when you’re talking about millions of users, it adds up. The effect is strongest with high-dose statins like atorvastatin 80 mg or rosuvastatin 40 mg. Lower doses still carry some risk, but it’s much smaller - around 10% higher than placebo.
At the biological level, statins block a pathway called the mevalonate pathway. This pathway doesn’t just make cholesterol - it also creates molecules like GGPP and CoQ10 that help insulin work properly. When these are reduced, glucose can’t enter your cells as easily. Your pancreas tries to compensate by pumping out more insulin, but over time, the beta cells get tired and start to fail.
Who’s Most at Risk?
Not everyone who takes statins will see their blood sugar rise. The risk is concentrated in people who already have signs of metabolic trouble. If you have any of these, you’re more likely to be affected:
- Prediabetes (fasting glucose between 100-125 mg/dL or HbA1c between 5.7%-6.4%)
- Obesity, especially around the waist
- High triglycerides and low HDL cholesterol
- High blood pressure
- Family history of type 2 diabetes
- Age over 65
- Taking other medications like steroids or diuretics
One study from Stanford found that people with metabolic syndrome - a cluster of these risk factors - had the clearest rise in blood sugar after starting statins. For someone with normal blood sugar and no other risk factors, the chance of developing diabetes from statins is tiny. But for someone with prediabetes and belly fat? The risk jumps noticeably.
Statins vs. Diabetes Risk: The Numbers
It’s easy to panic when you hear “statins cause diabetes.” But context matters. Here’s what the data really says:
For every 1,000 people taking a high-intensity statin for five years:
- 15-20 major heart attacks or strokes are prevented
- 1-2 additional cases of type 2 diabetes occur
That’s a 10-to-1 benefit-to-risk ratio. Even the American Heart Association and American Diabetes Association agree: for people who need statins for heart protection, the upside far outweighs the downside.
But here’s the catch: that math flips if you don’t actually need the statin. If you’re young, healthy, with borderline cholesterol and no other heart risks, the benefit is tiny - maybe 1 or 2 fewer heart events over five years. In that case, the diabetes risk might tip the scales. That’s why doctors now screen for prediabetes before prescribing high-dose statins.
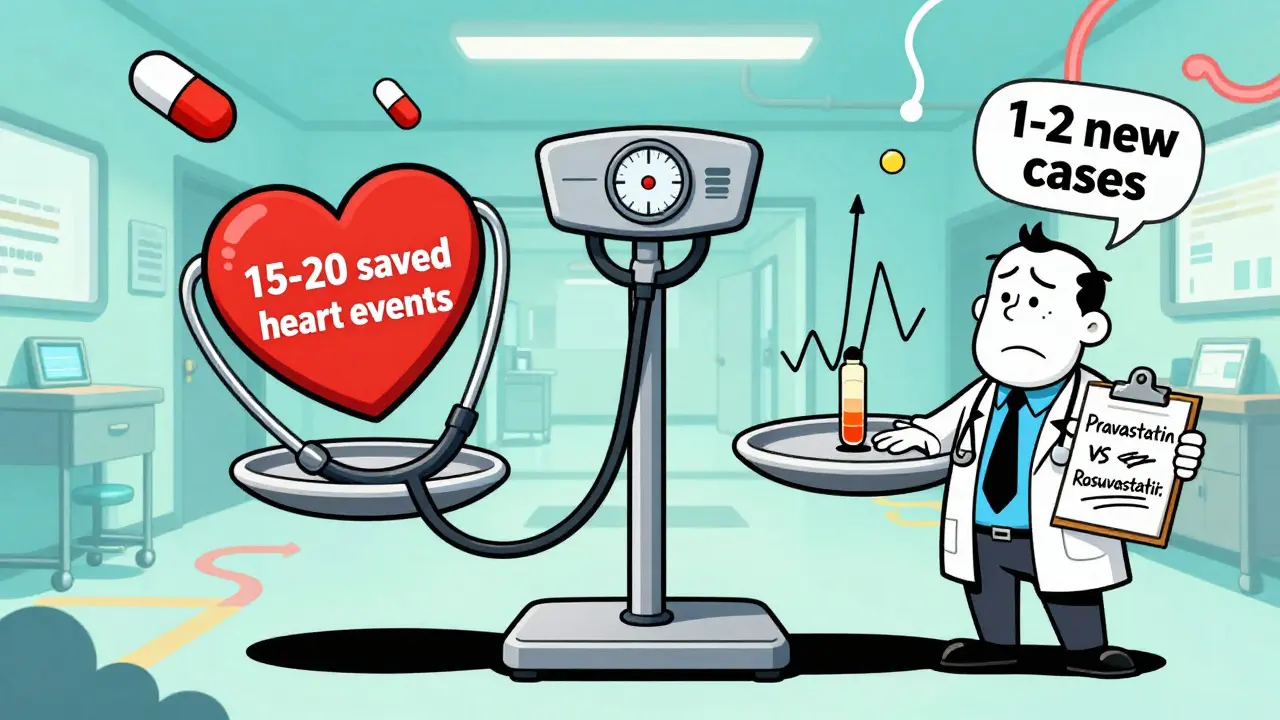
Which Statins Carry the Highest Risk?
All statins can raise blood sugar, but some do it more than others. The risk follows a clear pattern based on potency:
| Statin | Dose | Intensity | Relative Diabetes Risk Increase |
|---|---|---|---|
| Pravastatin | 40 mg | Low | +10% |
| Fluvastatin | 80 mg | Low | +12% |
| Atorvastatin | 10 mg | Low | +15% |
| Atorvastatin | 80 mg | High | +36% |
| Rosuvastatin | 40 mg | High | +36% |
For most people, the difference between a low- and high-intensity statin isn’t just about cholesterol lowering - it’s also about how much your blood sugar might climb. If you’re already at risk for diabetes, your doctor might choose a lower-intensity statin like pravastatin or fluvastatin. These still reduce heart risk significantly but with less metabolic impact.
What to Do If You’re on Statins
If you’re taking a statin and worried about blood sugar, here’s what actually helps:
- Get tested. Ask for a fasting glucose and HbA1c test before starting, and again at 3-6 months. If your numbers rise, don’t panic - but do talk to your doctor.
- Focus on lifestyle. Weight loss, even 5-10% of body weight, can reverse insulin resistance. Walking 30 minutes a day, five days a week, cuts diabetes risk by over 50% in statin users. Cutting sugary drinks and refined carbs helps too.
- Don’t stop your statin. Stopping statins because of blood sugar concerns is dangerous for people with heart disease or high risk. The chance of a heart attack or stroke jumps sharply if you quit.
- Consider alternatives. If you’re young, healthy, and on a high-dose statin just because your LDL is borderline, talk to your doctor about whether you really need it. Ezetimibe or PCSK9 inhibitors are alternatives that don’t raise blood sugar.
Some people report needing to start or increase metformin after beginning statins. That’s not unusual. It’s not a failure - it’s just your body adjusting to a new stressor.

Is the Effect Reversible?
Yes - in many cases, the blood sugar rise from statins can be reversed. Studies show that when people stop taking statins, insulin sensitivity improves within weeks. HbA1c levels often drop back down, especially if they’ve made lifestyle changes.
But again: stopping statins should only happen under medical supervision. If you have a history of heart attack, stroke, or very high cholesterol, the risks of stopping far outweigh the benefits of lowering blood sugar. For people who developed diabetes *because* of statins, the condition may persist even after stopping - but it’s often manageable with diet, exercise, and sometimes metformin.
What’s New in 2026?
Doctors are now looking at genetics to predict who’s most likely to develop statin-induced diabetes. A gene called SLCO1B1, which affects how statins are processed in the liver, has been linked to higher diabetes risk. In the future, a simple blood test might tell you whether you’re genetically more sensitive to this side effect.
Meanwhile, researchers are testing new statin-like drugs that lower cholesterol without blocking the mevalonate pathway as much. These could offer the heart benefits without the blood sugar trade-off. But they’re still years away from being widely available.
For now, the message is clear: statins save lives. The small increase in diabetes risk shouldn’t scare you away - but it should make you smarter about how you take them.
Bottom Line
Statins can raise blood sugar - especially high-dose ones - and push some people with prediabetes into diabetes. But for the vast majority of people who need them, the heart protection they offer is worth the risk. If you’re at risk for diabetes, get tested before and during treatment. Focus on diet and movement. Don’t stop your statin without talking to your doctor. And remember: this isn’t a reason to avoid statins. It’s a reason to use them wisely.
Do statins cause diabetes?
Statins don’t cause diabetes in healthy people. But they can push people with prediabetes or metabolic risk factors over the edge into type 2 diabetes. The increase in blood sugar is small - typically a 0.1% to 0.3% rise per year - but enough to cross the diagnostic threshold in vulnerable individuals.
Which statin is least likely to raise blood sugar?
Pravastatin and fluvastatin carry the lowest risk of raising blood sugar. These are lower-intensity statins, meaning they lower cholesterol less aggressively but also have less impact on insulin sensitivity. For people at high risk for diabetes, doctors often choose these over high-dose atorvastatin or rosuvastatin.
Should I stop taking statins if my blood sugar rises?
No - not without talking to your doctor. The cardiovascular benefits of statins are strong and proven. For people with heart disease or high risk, stopping statins increases the chance of a heart attack or stroke more than the risk from higher blood sugar. Instead, work with your doctor to adjust your diabetes management plan - diet, exercise, or medication - while staying on your statin.
Can lifestyle changes reduce the diabetes risk from statins?
Yes - significantly. Losing 5-10% of your body weight, walking 150 minutes a week, and cutting out sugary drinks and processed carbs can cut your diabetes risk by more than half, even while taking statins. Lifestyle changes are the most effective way to counteract the metabolic side effects.
How often should I check my blood sugar if I’m on statins?
If you have no diabetes risk factors, a baseline HbA1c test before starting statins is usually enough. If you have prediabetes, obesity, or other risk factors, get tested before starting, then again at 3-6 months, and annually after that. Monitoring is simple, cheap, and can catch changes early.

Statins are a necessary evil. I’ve seen too many people stop them because of fear-mongering online and then end up in the ER with a heart attack. The diabetes risk is tiny compared to the lifesaving benefits. If your blood sugar creeps up, manage it with diet and movement - don’t throw out the baby with the bathwater.
Doctors aren’t pushing statins for profit. They’re pushing them because the data doesn’t lie.
Stop treating medical advice like a TikTok trend.
So let me get this straight - a drug that causes diabetes is considered ‘worth it’ because it prevents heart attacks? That’s not medicine, that’s a gamble with your body’s long-term health.
And why are we still using statins when we know they mess with insulin pathways? Maybe the real problem is that we’re treating symptoms instead of causes - like diet, stress, inactivity.
Pharma loves this. You get a lifelong prescription for metformin, then another for blood pressure, then another for… you get the picture.
Thank you for this thoughtful, well-researched breakdown. I’m a nurse in rural Ohio, and I see this exact scenario every week - patients terrified of statins, or conversely, taking them without understanding the trade-offs.
One of my patients, a 68-year-old woman with prediabetes and a family history of heart disease, started on atorvastatin 80 mg. Her HbA1c went from 5.9 to 6.6 in six months. We switched her to pravastatin 40 mg, and within four months, her numbers dropped back to 5.8. She’s been walking daily, cutting out soda, and now she’s proud of her progress.
It’s not about avoiding statins. It’s about personalizing care. One size does not fit all - especially when metabolism is involved.
Also, thank you for mentioning SLCO1B1. Genetic testing for statin sensitivity is coming, and it’s long overdue.
It is interesting to note that the so-called 'benefit-to-risk ratio' of 10:1 is derived from population-level statistics, which are often misapplied to individual clinical decision-making.
One must question the source of the data: are these studies industry-funded? Are the control groups adequately matched? Is the definition of 'prediabetes' being expanded to inflate perceived risk?
Furthermore, the notion that 'the heart protection outweighs the diabetes risk' assumes a linear, deterministic model of human physiology - one that ignores the complexity of metabolic adaptation, epigenetic factors, and individual variability.
One might reasonably argue that the medical establishment has become overly reliant on pharmacological intervention at the expense of foundational lifestyle medicine.
It is not fear of statins that is irrational - it is the uncritical acceptance of their universal benefit.
YES. THIS. 🙌
I started statins after my first heart scare and my sugar went up. I panicked. But my doc said: 'Let’s fix your diet first.' I cut out the juice, started walking, lost 12 lbs. My HbA1c went down. I’m still on a low-dose statin. No metformin needed.
You don’t have to choose between heart and sugar. You just have to show up for yourself.
Also - pravastatin is a gem. My grandma’s on it and she’s 82 and still gardening. 💪
Statins are not the enemy. Complacency is.
If you’re on a statin and not moving, not eating real food, not sleeping - you’re setting yourself up for failure. The drug isn’t making you diabetic. Your lifestyle is. The statin just exposed the weakness.
Don’t blame the medicine. Fix the habits.
And if you think walking 30 minutes a day is too much? Then maybe you’re not ready to be healthy. That’s okay. But don’t pretend the pill is the problem.
So… let me get this straight - we give people a drug that makes them more likely to get diabetes… and then we tell them to eat less sugar and walk more… to fix the side effect of the drug we just gave them?
That’s not healthcare. That’s a joke. A really expensive, bureaucratic, corporate joke.
Who designed this system? Someone who’s never eaten a real meal? Someone who thinks 'lifestyle change' is just a hashtag?
Also - why are we still using 1980s science to treat 2020s bodies?
😂
I’m 52, prediabetic, on pravastatin 40mg. My doctor tested me before and after - my HbA1c went from 5.8 to 5.9. No big deal.
I started doing yoga three times a week, stopped eating cereal for breakfast, and now I feel better than I have in years.
Statins didn’t ruin my health - my stress and sugar addiction did.
And honestly? I’m grateful the statin gave me the nudge to finally change.
❤️
My dad’s on a high-dose statin after his bypass. His sugar went up a little, but his cholesterol is under control and he’s still hiking every weekend.
He didn’t stop the statin. He just started eating more veggies and walking after dinner.
It’s not an either/or. It’s a both/and.
Thanks for the clear info - I’ll share this with my mom. She’s scared to start hers.
The medical establishment has, for decades, prioritized pharmaceutical intervention over the fundamental principles of preventive medicine.
It is not merely coincidental that the rise in statin prescriptions parallels the explosion of type 2 diabetes in the Western world.
The mevalonate pathway is not a mere biochemical curiosity - it is a cornerstone of cellular metabolism. To disrupt it for the sake of cholesterol reduction is to engage in therapeutic hubris.
One must ask: who benefits? The patient? Or the shareholder?
And yet - the public, conditioned by advertising and paternalistic guidance, accepts this as inevitable.
It is not wisdom. It is surrender.
I keep thinking about how we treat the body like a machine you can tweak with one dial - lower cholesterol, fix heart, done.
But the body isn’t a car. It’s a forest. You can’t just cut one tree and expect the ecosystem to stay balanced.
Statins lower cholesterol - sure. But they also mess with CoQ10, which affects energy in every cell. That’s why some people feel wiped out on them.
And now we’re adding diabetes on top? It’s like patching a leak with duct tape while the whole roof is rotting.
Maybe we need to ask: why is the roof rotting in the first place?
Just saying.
Real talk: if you’re on a statin and your blood sugar is rising, don’t panic - but don’t ignore it either.
Get your HbA1c. Get your fasting glucose. Track your meals. Walk after dinner. Sleep better.
Most people don’t realize how much control they actually have - even while on meds.
And if your doctor doesn’t care to check your sugar? Find a new one.
Statins save lives - but only if you’re being monitored. This isn’t a set-it-and-forget-it drug. It’s a partnership.
You’re not a patient. You’re a partner in your health.
And you deserve better than a script and a shrug.
Statins cause diabetes? LOL. They also cause muscle pain, memory loss, and liver damage. But the FDA doesn't care. Big Pharma owns them. Your doctor gets kickbacks. Your sugar goes up? That's just a side effect of the system.
They want you addicted to pills. Not healthy.
Drink lemon water. Stop eating bread. You don't need statins. You need to stop lying to yourself.
They don't want you to know this. But now you do.