If you have allergies and keep getting sinus infections, you’re not alone. Many people with hay fever or dust mite allergies end up stuck in a cycle: sneezing, congestion, then a sinus infection that won’t go away. It’s not just bad luck-it’s biology. Allergies don’t just make your nose run; they inflame the lining of your sinuses, trapping mucus and creating the perfect environment for bacteria to grow. And when that inflammation sticks around for weeks or months, it becomes chronic sinusitis. Treating this isn’t about popping more antibiotics. It’s about breaking the cycle-and knowing when you need help beyond your primary care doctor.
Why Allergies Make Sinusitis Worse
Allergic rhinitis and chronic sinusitis are closely linked. Up to 70% of people with chronic sinusitis also have allergies. When you breathe in pollen, mold, or pet dander, your immune system overreacts. That triggers swelling in your nasal passages and sinuses. Swelling blocks the tiny drainage channels. Mucus builds up. Bacteria multiply. What starts as a simple cold turns into a sinus infection that won’t clear. The problem? Standard cold treatments don’t fix the root cause. Antibiotics might help if there’s a bacterial infection, but they do nothing for the underlying allergy. That’s why so many people keep coming back-same symptoms, same treatment, same results. Without controlling the allergy, the inflammation returns as soon as you stop the meds.First-Line Treatments That Actually Work
The most effective starting point isn’t a pill. It’s a spray and a rinse. Nasal corticosteroids are the gold standard. Fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) reduce swelling and mucus production directly where it’s happening. You won’t feel better right away. It takes 2 to 4 weeks of daily use to see real improvement. But once they kick in, they cut symptoms by 65% or more. That’s far better than oral antihistamines like cetirizine, which only help about 42% of the time. Saline nasal irrigation is just as important. Using a neti pot or squeeze bottle with distilled or boiled water (never tap water) flushes out allergens, mucus, and irritants. Do it once or twice a day. Studies show this simple step reduces sinus infections by up to 50% in people with allergies. The CDC warns: using unsterilized water can lead to rare but deadly brain infections from Naegleria fowleri. Always use sterile water-boil it for 1 minute and let it cool, or buy distilled.When Antibiotics Are (and Aren’t) Needed
Antibiotics are overused in sinusitis. For most people with acute sinusitis under 10 days, they’re unnecessary. But if you have allergies, the rules change. Your sinuses are already inflamed, so even a small bacterial push can trigger a full-blown infection. If symptoms last longer than 10 days, get worse after improving, or include high fever and thick yellow-green mucus, antibiotics may help. Amoxicillin is the first choice-500mg three times a day for 5 to 10 days. For stubborn cases, doctors may switch to amoxicillin-clavulanate. But here’s the catch: in allergy-related sinusitis, antibiotics alone work only 35-45% of the time. That’s half the success rate of bacterial sinusitis without allergies. The bottom line? Antibiotics treat the infection, not the allergy. They’re a band-aid unless you’re also treating the inflammation.
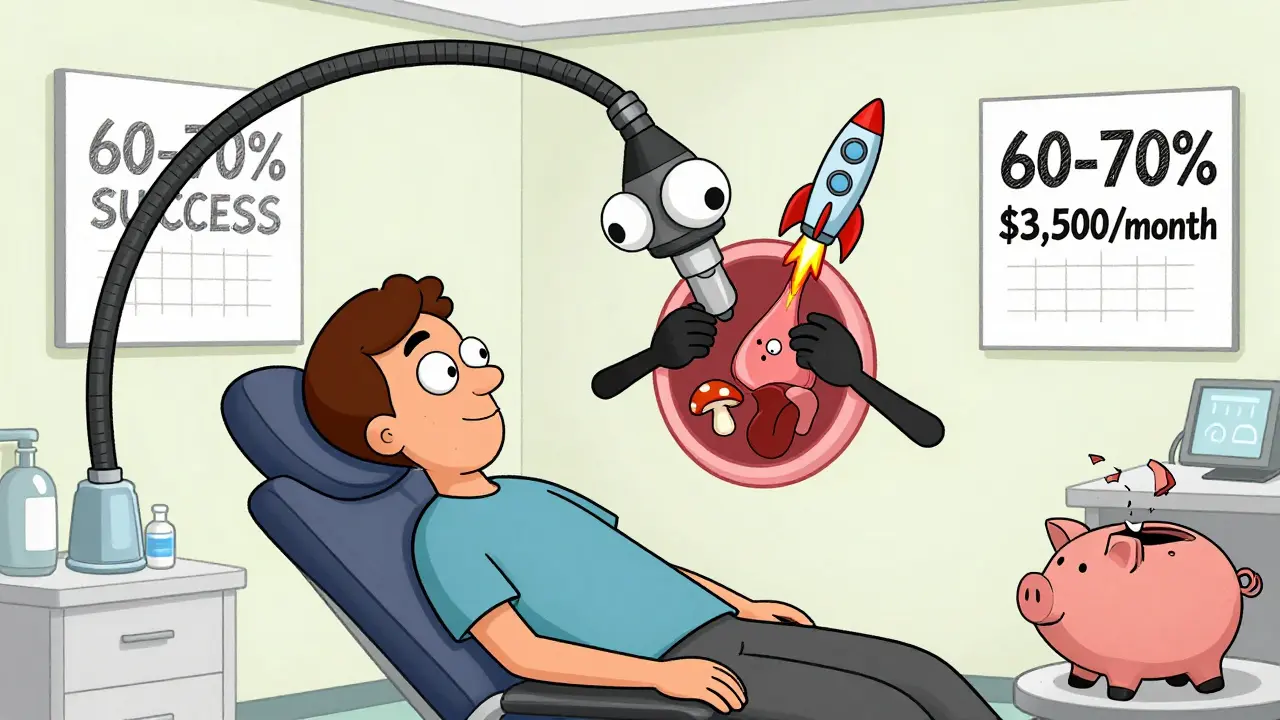
Long-Term Solutions: Immunotherapy and Biologics
If you’re stuck in a loop of sinus infections every few months, it’s time to think long-term. Allergy immunotherapy (allergy shots or tablets) reprograms your immune system. Over 3 to 5 years, you get regular doses of the allergens you react to. Your body learns not to overreact. Studies show this cuts sinusitis recurrence by 60-70%. That’s better than any medication. But it’s a commitment: weekly shots for months, then monthly for years. It’s not fast, but it’s the only treatment that can change your long-term health trajectory. For those with nasal polyps and severe, persistent symptoms, biologics are a game-changer. Dupilumab (Dupixent) is approved for chronic sinusitis with nasal polyps. It blocks key inflammation signals. In trials, it reduced polyp size by 73% and cut flare-ups by more than half. Omalizumab (Xolair) and mepolizumab (Nucala) are also options. But they cost around $3,500 a month without insurance. Most insurers require failure of at least two other treatments before approving them.When to See an ENT Specialist
You don’t need to wait until you’re desperate. See an ear, nose, and throat (ENT) doctor if:- Your symptoms haven’t improved after 4 to 6 weeks of proper treatment
- You have nasal polyps (seen on exam or imaging)
- You get 4 or more sinus infections a year
- You have complications like eye swelling, vision changes, or severe headaches
- You suspect fungal sinusitis (common in mold-prone areas)
What You Might Not Know About Aspirin and Mold
Some people with chronic sinusitis and polyps have a hidden trigger: aspirin sensitivity. Called aspirin-exacerbated respiratory disease (AERD), it affects 10-15% of this group. These patients can’t take NSAIDs like ibuprofen or aspirin without triggering severe congestion and asthma. They need specialized care, including aspirin desensitization under strict supervision. In damp climates or homes with poor ventilation, mold exposure is another silent culprit. The latest guidelines from January 2024 suggest using intranasal antifungals for allergy sufferers in high-mold environments. While not a cure, it can reduce symptom severity by 32% in some cases.Why Most People Fail at Treatment
The biggest reason sinusitis keeps coming back? People stop treatment too soon. Nasal sprays take weeks to work. Many quit after 2 weeks because they don’t feel better. Studies show only 35-40% of people are still using their nasal steroid after a month. Saline rinses? People skip them when they feel fine. But that’s when you need them most-to prevent the next flare-up. Also, many don’t address their environment. If you’re allergic to dust mites but don’t use allergen-proof bedding or run a HEPA filter, you’re fighting a losing battle. Environmental control-keeping humidity low, washing bedding weekly in hot water, removing carpets-can reduce symptoms by 40-60%.The Bigger Picture: Cost, Access, and Future Hope
Sinusitis costs the U.S. healthcare system over $3.5 billion a year. Allergy-related cases make up 30-40% of that. The new biologics are effective, but they’re out of reach for many. Insurance hurdles, high co-pays, and lack of specialist access mean rural patients wait 30-40% longer for referrals than city dwellers. The future is promising. Tezepelumab (Tezspire), approved in 2023, shows strong results for severe cases. Research into microbiome therapies-using good bacteria to crowd out bad ones-could cut antibiotic-resistant cases by nearly half in the next five years. But for now, the best tools are simple: nasal steroids, saline rinses, allergen avoidance, and knowing when to ask for help. You don’t have to live with constant congestion. There’s a path out-and it starts with treating the allergy, not just the infection.Can allergies cause chronic sinusitis?
Yes. Allergies trigger inflammation in the nasal passages and sinuses, which blocks drainage and leads to mucus buildup. This creates the perfect environment for infection and persistent swelling. Up to 70% of people with chronic sinusitis have underlying allergies.
Are antibiotics effective for allergy-related sinusitis?
Antibiotics help only if there’s a bacterial infection, which happens in about 0.5-2% of cases. In allergy-triggered sinusitis, antibiotics alone work in only 35-45% of cases-much lower than for regular bacterial sinusitis. They don’t fix the underlying allergy, so symptoms usually return.
How long do nasal steroid sprays take to work?
It takes 2 to 4 weeks of daily use to see full benefits. Many people stop too soon because they don’t feel immediate relief. Consistency is key-missing doses reduces effectiveness. Don’t expect instant results, but stick with it.
Is saline irrigation safe?
Yes, if done correctly. Always use distilled, sterile, or previously boiled (and cooled) water. Tap water can contain harmful microbes like Naegleria fowleri, which can cause rare but deadly brain infections. Use a neti pot or squeeze bottle with the right saline solution-once or twice daily.
When should I see an ENT specialist?
See an ENT if your symptoms don’t improve after 4-6 weeks of proper treatment, if you have nasal polyps, if you get 4 or more sinus infections a year, or if you have complications like eye swelling, vision changes, or severe headaches. Endoscopy can reveal issues your primary doctor can’t see.
Can allergy shots prevent sinusitis?
Yes. Allergy immunotherapy (shots or tablets) reduces sinusitis recurrence by 60-70% over 3-5 years. It works by training your immune system to stop overreacting to allergens. It’s the only treatment that can change your long-term risk-not just manage symptoms.
Do I need to avoid aspirin if I have sinusitis and polyps?
Some people with chronic sinusitis and nasal polyps have aspirin-exacerbated respiratory disease (AERD). If you get severe congestion or asthma after taking aspirin or ibuprofen, you may have this condition. It affects 10-15% of this group and requires specialized care, including aspirin desensitization under medical supervision.

Wow, someone actually got it right for once. Most people think antibiotics are magic bullets-nope. Allergies are the real villain here. You spray, you rinse, you stop being lazy. That’s it. No magic. No hype. Just discipline. And if you’re using tap water in your neti pot? You’re basically playing Russian roulette with your brain. Stop it.
This is the kind of info I wish my doctor had given me three years ago. I used to pop antibiotics like candy and wonder why it kept coming back. Started the nasal spray and saline rinse-didn’t believe it at first, but after six weeks? I forgot what it felt like to wake up congested. It’s not sexy, but it works. Stick with it.
Saline rinses changed my life. I used to think they were for hippies until I tried them. Now I do it every night before bed. No more waking up with my sinuses screaming. Also, HEPA filter + washing sheets in hot water? Non-negotiable. I wish more people knew how simple this stuff is.
Oh, so now we’re blaming the patient for not being disciplined enough? Brilliant. Let’s ignore that most people can’t afford $3,500/month biologics, or that their landlord won’t fix the moldy apartment, or that they work two jobs and don’t have time to boil water for a neti pot. Real helpful, genius. Meanwhile, the system is rigged. And you’re just here to shame people for being broke.
Just wanted to say-this post gave me hope. I’ve been stuck in this cycle for years. I thought I was just unlucky. Turns out I just needed the right tools. Started the spray and rinse last month. Still waiting on results, but I’m actually sticking with it. That’s huge for me. Thanks for the clarity.
Let me tell you something about India and this stuff-my uncle in Delhi had chronic sinusitis for 15 years, tried every pill, every injection, every Ayurvedic paste you can imagine. Nothing worked. Then his daughter, who works in Boston, sent him a neti pot and a bottle of distilled water. He started rinsing every morning. Within three months, he stopped taking antibiotics entirely. No drama. No fancy meds. Just clean water and consistency. People in the U.S. think they’re advanced, but sometimes the simplest solutions come from the most unexpected places. Don’t underestimate the power of a little water and a little patience.
Biologics aren’t a cure-they’re a luxury. And if your insurance denies them after you’ve tried everything else, you’re just out of luck. This whole system is broken. We treat symptoms like a checklist, not people. And then we act surprised when people give up. The real problem isn’t the allergy-it’s the healthcare system that makes effective care feel impossible.
It’s astonishing how many people still think ‘natural remedies’ are sufficient for a biological condition. Saline rinses? Cute. But if you’re relying on them while ignoring immunotherapy or biologics, you’re not being proactive-you’re being dangerously naive. This isn’t a yoga retreat; it’s immunology. And if you can’t afford Dupixent? Then you’re simply not in the same league as those who can. The world isn’t fair. Get over it.
Interesting. You mention that 70% of chronic sinusitis patients have allergies-but you don’t mention the converse: that 30% don’t. That’s a significant minority. Are we assuming all cases are allergy-driven? What about anatomical obstructions? Fungal etiologies? Autoimmune contributors? The article reads like a pamphlet from a pharmaceutical rep rather than a nuanced clinical overview. A more balanced perspective would acknowledge complexity, not reduce it to a single narrative.
As a physician practicing in rural Nebraska, I can confirm: access to ENT specialists is abysmal. Patients wait six to eight months for an appointment. Many never get one. We prescribe nasal steroids, recommend saline rinses, and urge allergen control-but without follow-up, without imaging, without endoscopy, we’re flying blind. The solution isn’t just better education-it’s better infrastructure. And that requires funding, policy, and political will. Not just a Reddit post.