Potassium Risk Calculator for ACE Inhibitors/ARBs
Your Risk Assessment
This tool calculates your risk of hyperkalemia when using potassium-based salt substitutes while taking ACE inhibitors or ARBs. Based on CDC and Mayo Clinic data.
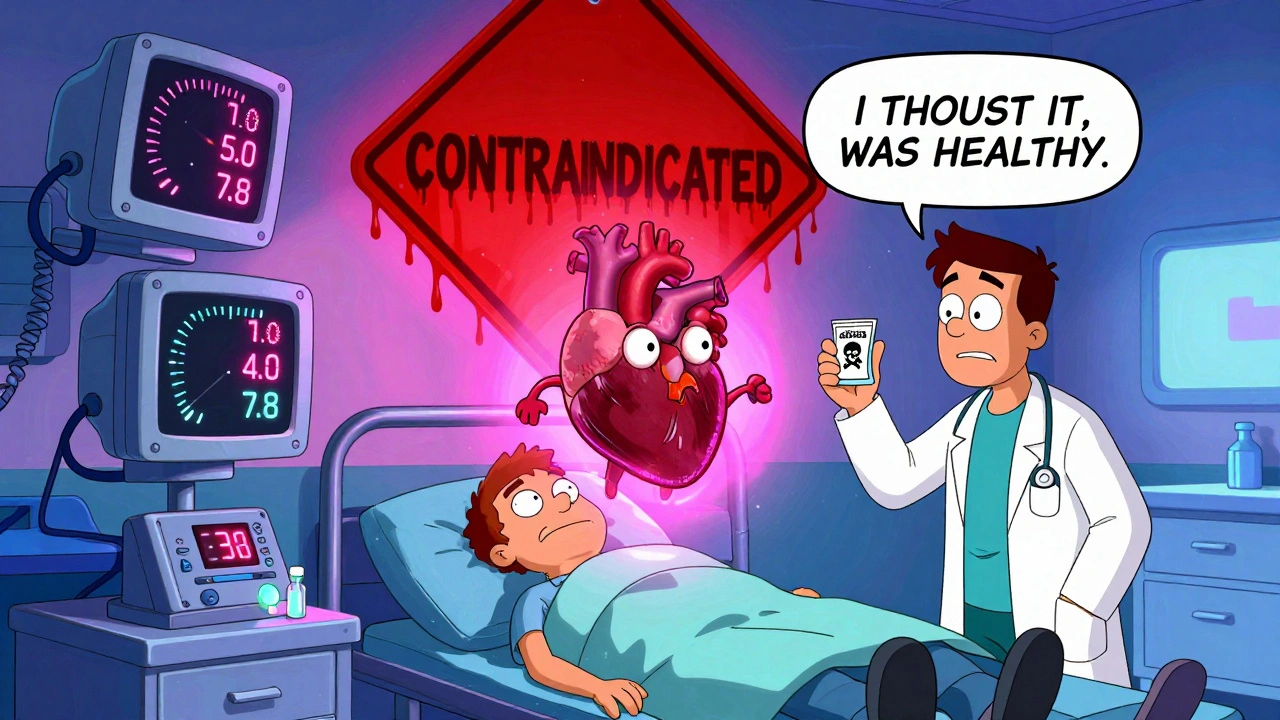
Many people switch to salt substitutes thinking they’re making a healthier choice-especially if they’ve been told to cut back on sodium. But for those taking ACE inhibitors or ARBs, that swap could be dangerous. It’s not just a minor concern. It’s a silent, life-threatening risk that doctors don’t always talk about-and patients rarely know about.
What’s in those salt substitutes?
Most salt substitutes don’t just remove sodium. They replace it with potassium chloride. Products like LoSalt, NoSalt, or Heart Salt often contain 50% to 66% potassium chloride. That means every teaspoon you use adds 400-600 mg of potassium to your diet. For someone with healthy kidneys, that’s usually fine. But for people on blood pressure meds like lisinopril, enalapril, losartan, or valsartan, it’s a different story.ACE inhibitors and ARBs work by blocking the renin-angiotensin-aldosterone system. That’s good for lowering blood pressure, but it also reduces aldosterone-a hormone that tells your kidneys to flush out excess potassium. So when you take these drugs, your body holds onto potassium. Add in a potassium-rich salt substitute, and your levels can climb fast.
Why this combo can be deadly
When potassium builds up in your blood, it’s called hyperkalemia. Normal levels are between 3.5 and 5.0 mmol/L. Once you hit 5.5 mmol/L, you’re in danger. At 6.5 mmol/L or higher, your heart can start beating irregularly-or stop entirely.A 2004 case report in the Journal of the Royal Society of Medicine documented a 72-year-old man who went into cardiac arrest after using LoSalt while taking nabumetone and already having mild kidney trouble. His potassium level hit 7.8 mmol/L. He survived, but only because he got emergency treatment. That’s not rare. In fact, a 2022 Mayo Clinic study found that 63% of hyperkalemia cases in people on ACE inhibitors or ARBs came from hidden dietary sources-not from supplements or kidney failure alone.
Who’s most at risk?
Not everyone is equally vulnerable. The biggest red flags:- You have chronic kidney disease (CKD), especially stage 3 or worse (eGFR below 60)
- You have diabetes with hyporeninemic hypoaldosteronism (affecting 10-20% of diabetics with kidney issues)
- You’re over 65 and on multiple medications
- You’ve had high potassium levels before
According to CDC data, 15% of U.S. adults have CKD. That’s about 37 million people. And 40% of hypertension patients are on ACE inhibitors or ARBs. That means millions are walking into this risk without knowing it.
Even if you feel fine, your kidneys might not be working as well as you think. An eGFR below 60 means your kidneys are struggling to clear potassium. The National Kidney Foundation says patients with eGFR under 45 should avoid potassium salt substitutes entirely. Those with eGFR between 45 and 60 need doctor approval before using them.
What do the studies say?
It’s not all bad news. A major 2025 study in JAMA Network Open followed 21,000 people for five years. Those using salt substitutes with 25% potassium chloride had a 14% lower risk of stroke. That’s huge. But here’s the catch: almost all of them had healthy kidneys. The benefits don’t apply to people with kidney disease.Another analysis from the Chronic Kidney Disease Prognosis Consortium looked at over 1.2 million people. In the general population, hyperkalemia from salt substitutes was rare-just 0.8 events per 100 person-years. But for those with CKD on ACE inhibitors or ARBs? That jumped to 8.7 events per 100 person-years. That’s more than ten times higher.
Real people, real consequences
Online forums are full of warnings. One Reddit user with 4,200 karma wrote: “Woke up in the ER with potassium at 6.3 after using ‘Heart Salt’ for three weeks while on lisinopril.” Another, Martha from Michigan, posted on Drugs.com: “Severe muscle weakness, irregular heartbeat. My doctor said I almost died.”These aren’t outliers. A 2023 Amazon review analysis showed 7% of users with self-reported kidney conditions said their doctor told them to stop the salt substitute after bloodwork showed high potassium. Meanwhile, 28% complained about a metallic aftertaste-proof that many people don’t even like the flavor, yet keep using it because they think it’s “healthy.”
What about herbs and spices?
You don’t need potassium chloride to cut sodium. Herbs, spices, lemon juice, garlic, vinegar, and no-salt blends like Mrs. Dash can reduce sodium intake by 40-50%-without touching potassium. That’s almost as good as salt substitutes, but without the risk.And they’re cheaper. Standard iodized salt costs about $1 per 12-ounce container. Potassium-based substitutes? $3 to $6. For people on fixed incomes, that’s a real barrier. But if you’re on ACE inhibitors or ARBs, the cost of a hospital visit or a heart rhythm problem is far higher.

Why aren’t we warned?
The labeling on these products is dangerously vague. A 2023 FDA review found only 3 out of 12 major brands clearly warn against use with ACE inhibitors or ARBs. Most say “low sodium” or “heart-healthy”-nothing about potassium. Canada changed its rules in January 2024: now, all potassium salt substitutes must say “Contraindicated in patients taking ACE inhibitors.” The U.S. hasn’t done that yet.The FDA proposed new labeling rules in May 2024, but they won’t be final until mid-2026. In the meantime, patients are being exposed to avoidable danger.
What should you do?
If you’re on an ACE inhibitor or ARB:- Check your current salt substitute. Look at the ingredients. If it says “potassium chloride,” stop using it.
- Ask your doctor for a blood test to check your potassium level. It’s a simple, cheap test.
- Ask your pharmacist: “Does this medication interact with potassium-rich foods or salt substitutes?”
- Switch to herbs and spices. Try smoked paprika, cumin, oregano, or a no-salt seasoning blend.
- If you still want to reduce sodium more aggressively, talk to a dietitian. They can help you cut sodium safely without potassium.
And if you’re a healthcare provider: screen every patient on ACE inhibitors or ARBs for salt substitute use. A 2023 JAMA Internal Medicine study found 78% of patients didn’t know dietary potassium could raise their risk. That’s not patient error-that’s a system failure.
The bottom line
Salt substitutes aren’t universally good or bad. For healthy people, they can help lower blood pressure and reduce stroke risk. But for the 10-15% of people with kidney problems or on certain blood pressure meds, they’re a ticking time bomb.There’s no need to panic. Just be informed. If you’re on an ACE inhibitor or ARB, don’t assume “low sodium” means “safe.” Check the label. Ask your doctor. And remember: flavor doesn’t have to come from potassium chloride. It can come from garlic, lime, or a pinch of black pepper. Your heart will thank you.

I used one of those salt substitutes for months thinking it was healthier. Woke up one morning with my arm numb and heart racing. ER said my potassium was 6.1. My doctor looked at me like I’d just confessed to stealing his lunch. Turns out I was on lisinopril. Never used it again. Just use garlic and chili now. So much better anyway.
This is an incredibly important post. The FDA’s delay in mandating clear labeling on potassium chloride products is negligent. Patients on ACE inhibitors and ARBs are being exposed to preventable risks because manufacturers prioritize marketing over safety. Clear, bold warnings should be required on every package. This isn’t just about education-it’s about accountability.
I’m telling you, if you’re on blood pressure meds and you’re using anything that says ‘heart-healthy’ on the label, you’re playing Russian roulette with your heart. I watched my uncle collapse at the dinner table because he thought ‘no sodium’ meant ‘no danger.’ He didn’t even know potassium chloride was in it. He’s lucky to be alive. This needs to be on every pharmacy poster.
The 2022 Mayo Clinic data is particularly alarming-63% of hyperkalemia cases linked to dietary sources, not supplements or renal failure. This suggests a systemic failure in patient counseling. Primary care providers are not asking about seasoning habits. Pharmacists aren’t flagging it during med reviews. And patients? They assume ‘low sodium’ equals ‘safe.’ We need standardized screening protocols. This isn’t a niche concern-it’s a public health blind spot.
i live in india and we use rock salt and black salt all the time. never heard of potassium chloride stuff. we just use cumin, coriander, lemon, and chilli. tastes better too. my uncle in texas used one of those fancy salts and ended up in hospital. i told him, why not just use real food? why buy poison in a jar?
So now we’re blaming salt substitutes? What about all the processed food companies that pump sodium into everything? This is just another distraction. If the FDA cared, they’d ban the junk food, not make people paranoid about a $5 salt substitute. You’re all missing the real problem.
I switched to Mrs. Dash after my doctor warned me and I’ve never looked back. It’s so easy to forget how much flavor you can get from herbs. I even make my own blend with smoked paprika and a little turmeric. Tastes like a party in my mouth and my potassium levels are perfect. You don’t need chemicals to be healthy.
I didn’t even know potassium chloride was in salt substitutes. I thought they were just ‘less salty.’ My mom’s on losartan and she’s been using LoSalt for years. I’m sending her this right now. Thanks for spelling it out so clearly. This is the kind of info that should be in every doctor’s office.
You’re all panicking over a mineral. Potassium is natural. Your body needs it. If your kidneys can’t handle it, maybe you’re the problem, not the salt substitute. Stop blaming products and start taking responsibility for your health.
I just bought a bag of this stuff last week 😳 I thought it was like sea salt but better? Now I’m scared to even breathe. Someone please tell me I’m not gonna die before my coffee gets cold.
Ah yes, the classic American medical tragedy: we’re told to reduce sodium, so we buy a product that replaces it with a different electrolyte we’ve never heard of, then act shocked when our heart goes on vacation. The real innovation here is our collective ability to ignore basic physiology while buying ‘heart-healthy’ marketing. Bravo.
This is all just fearmongering. I’ve been using potassium salt for 10 years. My doctor says I’m fine. You’re just trying to scare people into buying expensive herbs. Also, garlic is overrated.
Of course the FDA is slow. They’re too busy protecting Big Pharma. This is just another way to profit off the sick. Who benefits from this panic? The companies selling ‘no-salt’ blends. The real villain is the medical-industrial complex. Don’t fall for it.
To the person who said ‘your kidneys are the problem’-that’s not just wrong, it’s dangerous. CKD is often asymptomatic until it’s advanced. Millions of people don’t know they have it. The burden shouldn’t be on patients to know every biochemical interaction between their meds and their seasoning. It’s the system’s job to warn them. This isn’t about blame-it’s about safety.