Switching from a brand-name drug to a generic version is one of the most common changes in your medication routine - and for good reason. Generics cost less, often by 80% or more, and they’re just as effective for most people. But if you’ve ever wondered whether you should be watching your body more closely after the switch, you’re not alone. The truth is, while generics are held to the same strict standards as brand-name drugs, some people do notice changes. Not because the generic is broken, but because your body is sensitive - and that’s okay.
Why You Might Notice Something Different
Generic drugs must contain the exact same active ingredient, strength, and dosage form as the brand-name version. The U.S. Food and Drug Administration (FDA) requires them to deliver the same amount of medicine into your bloodstream within the same time frame. That’s called bioequivalence. For most drugs, this works perfectly. In fact, over 90% of prescriptions filled in the U.S. are generics, and most people never notice a difference. But here’s the catch: generics can have different inactive ingredients. That means the fillers, dyes, or coatings might be different. For most people, that’s harmless. But if you’re sensitive to certain dyes, or if your body reacts to small changes in how the medicine is absorbed, you might feel it. This isn’t about quality - it’s about individual biology. Some medications are especially tricky. Drugs with a narrow therapeutic index - like warfarin, levothyroxine, lamotrigine, or certain seizure meds - mean there’s a very small range between the dose that works and the dose that causes problems. Even tiny shifts in how your body absorbs the drug can affect how you feel. That’s why doctors often recommend extra monitoring for these.What to Track After the Switch
You don’t need to panic. But you do need to pay attention for the first few weeks. Here’s what to watch, depending on your condition:- Thyroid medication (levothyroxine): Watch for fatigue, weight changes, heart palpitations, or mood swings. Get your TSH level checked at 4 and 8 weeks after switching.
- Antiseizure drugs (lamotrigine, phenytoin): Keep a seizure diary. Note frequency, duration, or intensity. If seizures become more frequent or new types appear, contact your doctor right away.
- Blood thinners (warfarin): Your INR levels must stay in a tight range. Get tested at 7 days and again at 30 days after switching. Don’t wait for symptoms - this is silent but dangerous.
- Diabetes (metformin, insulin): Track your fasting blood sugar and HbA1c. If your levels start creeping up without changes to diet or activity, it could signal a problem.
- High blood pressure or heart meds: Check your blood pressure at home twice a week for the first month. If your readings become erratic or your symptoms (dizziness, chest tightness) return, don’t ignore it.
- Antidepressants (bupropion, SSRIs): Mood shifts, sleep changes, or increased anxiety in the first 2-4 weeks could be a sign your body isn’t adjusting well.
How to Keep a Simple Medication Diary
You don’t need a fancy app. A notebook or even a notes app on your phone works. Write down:- What time you took your pill each day
- Any new or worsening symptoms (headache, nausea, dizziness, mood changes)
- Any changes in how you feel - energy, sleep, focus, appetite
- Relevant numbers: blood pressure, blood sugar, seizure count, INR, TSH
Check the Label - NDC and Lot Numbers Matter
Not all generics are made the same. Different companies make the same drug, and even small differences in manufacturing can affect how it works for you. Always check the National Drug Code (NDC) on your pill bottle. It’s a 10- or 11-digit number. If it changes from one refill to the next, that’s a different manufacturer. That’s normal - but if you start feeling worse after a change, it might be worth mentioning. Also, keep the lot number. If you have a bad reaction, that number helps trace the batch. The FDA uses this to spot patterns. If 10 people report the same issue with the same lot, they investigate.
When to Call Your Doctor
You don’t need to call at the first sign of a headache. But if you notice any of these, reach out:- Symptoms return or get worse after switching
- New side effects you didn’t have before
- Lab results (INR, TSH, blood sugar) move outside your normal range
- You feel like the medication isn’t working like it used to
What to Do If You Think Something’s Wrong
If you believe your generic medication isn’t working or is causing harm, report it. The FDA’s MedWatch program is designed for exactly this. You don’t need to be a doctor. Just go to www.fda.gov/medwatch or call 1-800-FDA-1088. When you report, give them:- Your name and contact info (optional but helpful)
- The name of the drug (brand and generic)
- The NDC and lot number
- When you started taking it
- What symptoms you had and when they started
The Numbers Don’t Lie - But Your Body Does
Studies show that 92-93% of people who switch to generics have no issues. That’s reassuring. But 7-8% do notice changes - and for a small fraction, those changes matter. In one survey of over 42,000 people, only 1.2% needed medical help after switching. That’s low. But if you’re in that 1.2%, it’s everything. The FDA, the World Health Organization, and medical groups like the American Academy of Family Physicians all agree: generics are safe. But safety doesn’t mean one-size-fits-all. Your body is unique. Monitoring isn’t distrust - it’s self-advocacy.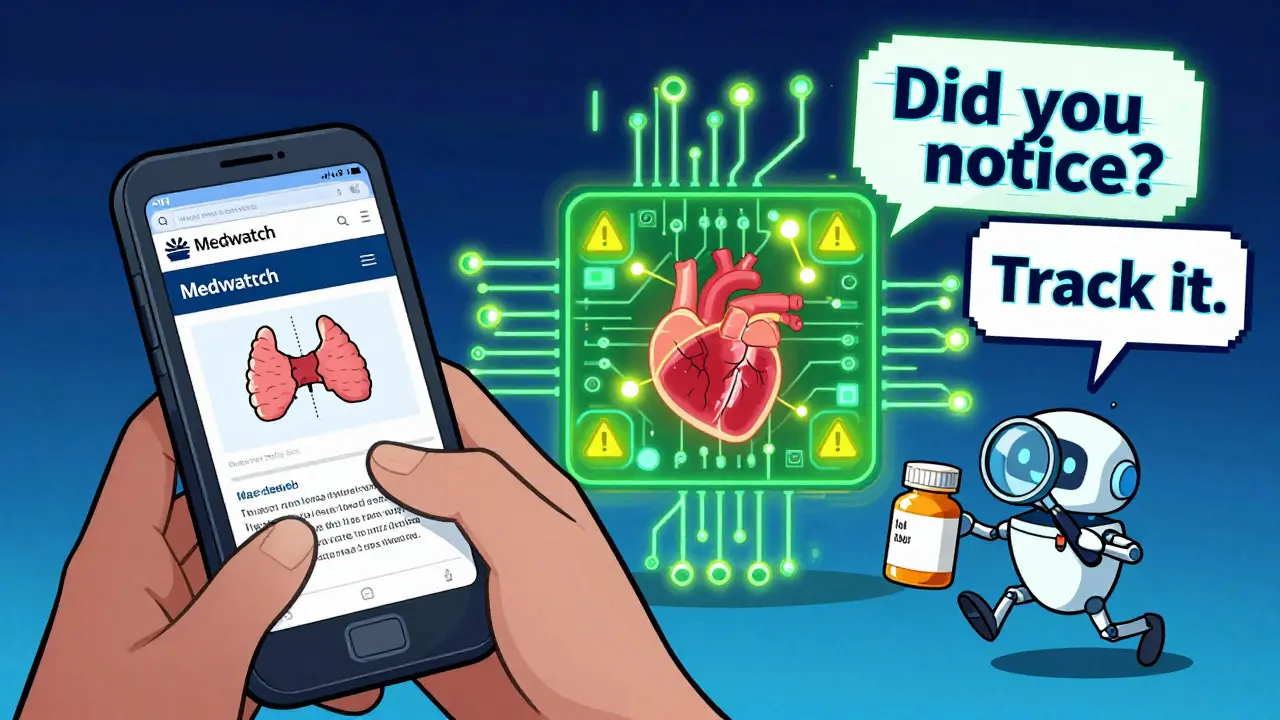
What’s Next for Generic Drugs?
The system is getting smarter. By 2025, the FDA plans to use artificial intelligence to scan every adverse event report linked to generics within 72 hours - down from the current 7 days. They’re also rolling out a national drug tracking system to trace every pill from factory to pharmacy. That means if a batch causes problems, they’ll find it faster. For now, your best tools are awareness, tracking, and communication. You don’t need to be an expert. Just be observant. Keep notes. Ask questions. Speak up.Frequently Asked Questions
Are generic drugs really as good as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. They’re tested in labs and clinical studies to prove they work the same way. Over 90% of prescriptions in the U.S. are generics, and they’ve saved the healthcare system over $370 billion since 2010. For most people, they’re just as effective.
Why do some people feel worse after switching to generics?
It’s usually not the active ingredient. It’s the inactive ones - fillers, dyes, coatings - that can affect how the drug is absorbed. People with sensitive systems, especially those on drugs with narrow therapeutic indices (like thyroid meds or seizure drugs), may notice differences in how they feel. That doesn’t mean the generic is bad - it just means your body responds differently to the formulation.
Which medications need the most caution when switching?
Drugs with a narrow therapeutic index are the most sensitive. These include levothyroxine (for thyroid), warfarin (blood thinner), lamotrigine and phenytoin (for seizures), digoxin (for heart), and some antidepressants like bupropion. For these, your doctor may recommend lab tests 1-4 weeks after switching to make sure levels are still in the safe range.
Should I ask my doctor before switching to a generic?
You don’t have to - pharmacists are allowed to substitute generics unless your doctor writes "dispense as written." But if you’re on a sensitive medication, it’s smart to ask. Say: "I’ve had good results with this brand. Is there a reason we should stick with it?" Most doctors will agree to keep you on the same version if you’ve been stable.
What if my pharmacy switches the generic without telling me?
It happens. Pharmacies often switch to the cheapest generic available. Always check the NDC number on your bottle. If it’s different from your last refill, you’ve got a new manufacturer. If you feel worse, call your pharmacy and ask why it changed. You have the right to request the same generic or the brand if needed.
Can I switch back to the brand-name drug if I’m not feeling well?
Yes. If you’ve noticed a clear decline in how you feel after switching, talk to your doctor. They can write a prescription for the brand-name version, often with a note like "do not substitute." Some insurance plans require prior authorization, but many will cover it if there’s documented medical need. Your health comes first.
Next Steps
If you just switched to a generic:- Write down the drug name, NDC, and lot number.
- Start a 30-day symptom tracker - even if you feel fine.
- Schedule a follow-up with your doctor if you’re on a high-risk medication.
- Don’t stop taking your medicine unless your doctor tells you to.
- Report any serious changes to the FDA via MedWatch.

I switched my levothyroxine last month and didn't think twice until I started crashing by 3pm. Got my TSH checked and it was off by 0.8. Pharmacist said it was the same generic but different manufacturer. Now I check the NDC every time. Don't let them fool you.
Oh wow so the FDA is just letting Big Pharma swap out your meds like a bad magic trick?? 😏
Wait till you find out the dye in your generic lamotrigine is the same as the one in that cereal that made 3 people hallucinate in 2019. They don't test the fillers, they just hope you're not allergic to cornstarch or existential dread. 🤡
This is such a thoughtful breakdown. I'm on warfarin and I've been tracking my INR religiously since switching generics. My numbers stayed rock solid, but I'm glad I did it anyway. Knowledge is power, even if the system doesn't always care.
YOU THINK THIS IS BAD??
Have you seen the batch recalls from 2021? The same lot of generic metformin that made people nauseous? It was shipped to 47 states and no one told you. The FDA doesn't care until 20 people die. You think your NDC matters? It's a lottery ticket with your life on it.
Oh please. In the UK, we’ve had generics for decades and no one’s dropping dead from a filler. Americans are so dramatic about pills it’s pathetic. You take your meds, you don’t keep a diary like you’re writing a novel. We don’t need 90 days of symptom tracking-we need to stop treating medicine like a cult.
Let’s deconstruct the epistemological fallacy embedded in the FDA’s bioequivalence paradigm.
When we reduce pharmacological efficacy to plasma concentration curves, we ontologically erase the phenomenological experience of the embodied patient.
The inactive ingredients aren’t inert-they’re semiotic signifiers of capitalist commodification, mediating your corporeal subjectivity through proprietary excipient matrices.
Levothyroxine isn’t just T4-it’s a neoliberal biopolitical apparatus disguised as a tablet.
Your ‘symptom tracker’? A Foucauldian panopticon of self-surveillance, incentivized by insurance-driven cost-cutting.
And don’t get me started on the NDC-it’s a barcode of alienation, reducing your biological uniqueness to a 10-digit commodity code.
Who benefits from your compliance? Not you. Not the FDA. Not even the manufacturer.
It’s the algorithm that optimizes profit margins by swapping your thyroid hormone for a cheaper dye.
Wake up. You’re not monitoring your health-you’re performing data for a system that doesn’t care if you live or die, as long as your INR stays in the spreadsheet.