When a life-saving medication has no generic version, the price can be crushing. Some drugs cost more than $10,000 a month. For many people, that’s not just expensive-it’s impossible. But there’s a lifeline: patient assistance programs (PAPs). These are free or low-cost drug programs run by drug companies, nonprofits, and sometimes states. They exist specifically for situations like this-when there’s no cheaper alternative. If you’re stuck paying full price for a brand-name drug with no generic, PAPs aren’t just helpful. They might be your only way to stay alive.
Why PAPs Matter When No Generic Exists
Generic drugs cut costs by 80% or more. But for many rare diseases, cancer treatments, and specialty medications, generics don’t exist. Drugs like Soliris, Tasigna, or certain HIV medications have no cheaper version. Their list prices? Often over $500,000 a year. Without help, patients choose between bankruptcy and skipping doses. That’s where PAPs step in. In 2022, these programs gave out $4.7 billion in free or discounted drugs. Most of that went to brand-name medications with no alternatives. About 78% of PAP funds went to patients who had no other options. These aren’t charity handouts-they’re structured support systems built into the system because the system itself doesn’t work for high-cost drugs.Who Qualifies for Patient Assistance Programs?
You don’t need to be poor to qualify. Most programs use income limits based on the Federal Poverty Level (FPL). For a single person in 2023, that meant earning less than $60,000 a year to qualify for full assistance. Some programs stretch even higher-up to 500% FPL for certain rare diseases. But income isn’t the only factor. You’ll usually need:- A valid prescription from your doctor
- Proof of income (tax returns, pay stubs, or W-2s)
- Proof of U.S. residency
- Verification that you don’t have insurance that covers the drug, or that your insurance denies it
How to Find the Right Program
There are over 1,500 PAPs in the U.S. Trying to find one on your own is like searching for a needle in a haystack. Start here:- Use RxHope-it’s a free online tool that checks 92% of manufacturer PAPs. Just enter your drug name and income. It tells you which programs you qualify for.
- Check the drug manufacturer’s website. Look for “Patient Assistance,” “Support Programs,” or “Help with Costs.” Most have a dedicated page.
- Call your pharmacy. They often have access to PAP databases and can guide you.
- Reach out to nonprofits like the Patient Advocate Foundation or NORD (National Organization for Rare Disorders). They offer free case management.
The Application Process: What to Expect
Applying for a PAP isn’t easy. It’s designed to be thorough. Most applications ask for:- 17+ fields of personal and financial info
- Three to four documents (tax forms, ID, prescription)
- A signed form from your doctor
- Get your doctor’s office to help. Most hospitals now have “medication access specialists” who handle PAP applications. Ask for them.
- Keep copies of everything. Submit everything by mail or online, but never rely on just one method.
- Apply early. Manufacturer programs take 7-10 days to approve. Foundations take 2-3 weeks.
- Don’t give up if you’re denied. About 41% of initial applications get rejected-but many are approved on appeal.
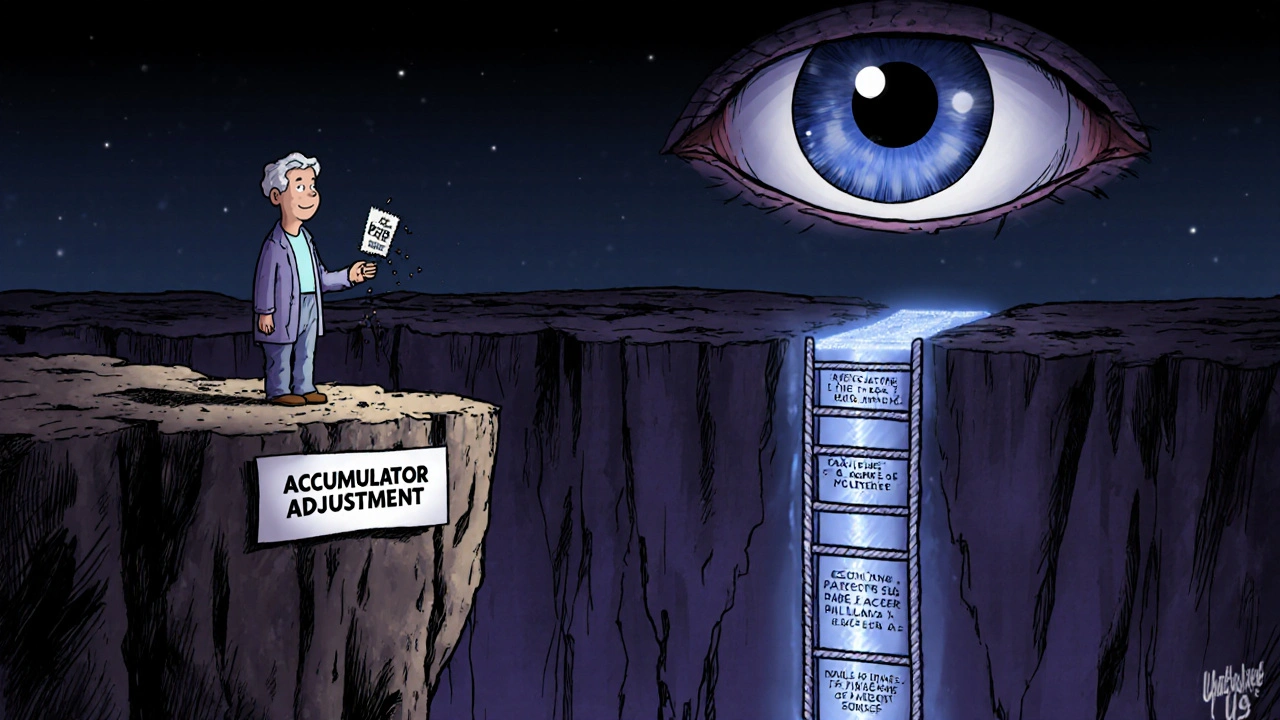
The Hidden Trap: Accumulator Adjustments
This is the part no one tells you. Even if you get approved for a PAP, your insurance might not count it toward your deductible or out-of-pocket maximum. This is called an “accumulator adjustment.” Here’s how it works: Your PAP covers your $12,000 monthly drug cost. You pay $0. But your insurance says, “That $12,000 doesn’t count toward your $8,000 deductible.” So next month, you still owe $8,000 out of pocket-even though you didn’t pay a dime for the drug. 78% of major insurers like UnitedHealthcare, Express Scripts, and Optum use this trick. It’s legal. And it ruins the whole point of PAPs for people with commercial insurance. Solution? If you have insurance, ask your insurer: “Do you have accumulator adjustments?” If yes, look for foundation-based PAPs. They’re not subject to these rules. Or ask your doctor to switch to a drug that’s covered under your plan’s formulary-even if it’s less ideal.PAPs vs. Other Help Options
You might hear about GoodRx coupons, state programs, or pharmacy discounts. Here’s how they stack up:| Option | Best For | Average Savings | Eligibility |
|---|---|---|---|
| Patient Assistance Programs (PAPs) | Brand-name drugs with no generic | Up to 100% off | Income-based, often requires no insurance or Medicare |
| GoodRx Coupons | Generic drugs or low-cost brand names | 52% average, but only 8% on specialty drugs | Anyone with or without insurance |
| State Pharmaceutical Programs (SPAPs) | Seniors on fixed income | Up to $400/month per drug | Age 65+, income under $28,500 (varies by state) |
| Nonprofit Foundations | Medicare patients or those with accumulator issues | Up to 100% off | Income-based, no manufacturer restrictions |
Real Stories: What Happens When You Get Help
One patient with HIV was paying $15,000 a month for his medication. He lost his job. His savings vanished. He applied to Gilead’s PAP. Approved. His monthly cost dropped to $0. He kept his apartment. He stayed on treatment. Another, with a rare blood disorder, was told she’d need $500,000 a year for her drug. Her doctor connected her with a nonprofit. She got full coverage. She didn’t have to sell her house. But it’s not always smooth. One Medicare patient spent three months fighting UnitedHealthcare’s accumulator policy. Even though her PAP covered her $12,000 drug, she still paid $20,700 out-of-pocket because the assistance didn’t count toward her deductible. The difference? Support. People who got help from a navigator-whether from their hospital, a nonprofit, or a pharmacist-had much higher success rates.What’s Changing in 2025?
New rules are coming. Starting January 1, 2025, Medicare Part D patients can no longer get copay help from drug manufacturers. That means more people will turn to nonprofit foundations. These groups are already overwhelmed. Some drug companies are making it easier. Eli Lilly’s “Simple Bridge” program cuts its PAP application from 17 steps to 5. Approval now takes 48 hours for insulin. Other companies are following. Hospitals are also hiring more patient navigators. In 2020, only 76% of U.S. hospitals had PAP support. By 2023, it was 98%. That’s a big win.What to Do Right Now
If you’re on a brand-name drug with no generic:- Go to RxHope.com. Enter your drug name and income. See what’s available.
- Call your doctor’s office. Ask if they have a medication access specialist.
- Check the drugmaker’s website. Look for “Patient Assistance” or “Support.”
- If you’re on Medicare, contact the Patient Access Network Foundation or the Chronic Disease Fund.
- Ask your insurer: “Do you use accumulator adjustments?” If yes, ask your doctor about alternatives.
- Apply immediately. Processing takes weeks. Don’t wait until your prescription runs out.
Can I use a patient assistance program if I have insurance?
Yes, but it depends. If you have commercial insurance, many PAPs still accept you-but your insurer may have an accumulator adjustment policy that blocks the assistance from counting toward your deductible. That means you could still owe thousands even with PAP help. If you’re on Medicare, you can’t use manufacturer PAPs, but nonprofit foundations can still help.
What if my PAP application is denied?
Don’t give up. About 41% of initial applications are denied-but many are approved on appeal. Review the denial letter. Did you miss a document? Is your income slightly over the limit? Call the program. Ask for help. Sometimes, a letter from your doctor explaining your medical need can change the outcome.
Do patient assistance programs cover all my medication costs?
Most manufacturer PAPs cover 100% of the drug cost if you qualify. Foundation programs often do too. But they usually don’t cover administration fees, lab tests, or doctor visits-just the drug itself. Always check what’s included before assuming.
How long does it take to get approved for a PAP?
Manufacturer programs typically approve applications in 7-10 business days. Foundation programs take longer-14 to 21 days-because they review more paperwork. Apply as soon as possible. Don’t wait until your prescription runs out.
Can I apply for multiple PAPs at once?
Yes. You can apply to multiple programs for the same drug, or for different drugs you’re taking. Some patients get help from both a manufacturer PAP and a nonprofit foundation. Just make sure you’re not violating any program rules-most allow multiple applications, but always confirm.

This post is a lifeline for people who are just one paycheck away from losing their medication. I’ve seen friends cry over $12,000 monthly bills for drugs that save their lives. No one should have to choose between rent and survival. The fact that these programs exist-and work-is a small miracle in a broken system. Please, if you’re reading this and you’re struggling, don’t wait. Apply today. Even if you get denied once, appeal. They’re not perfect, but they’re the only thing standing between you and disaster.
And if you’re lucky enough to have access to this info, share it. Someone you know might be silently drowning.
USA is so f***ed up. In India we dont have these crazy prices. Even cancer drugs cost 1/10th here. But no one in US wants to fix the system they just cry about it. Pharma companies are robbers. They charge 10000$ for a pill that costs 2$ to make. Why dont you all protest? Why dont you burn down their offices? You just sit there and apply for paps like its some kind of charity. Its a crime.
While I appreciate the intent of this article, it fails to address the systemic moral hazard created by permitting pharmaceutical companies to operate without price regulation. The existence of patient assistance programs does not mitigate the ethical failure of pricing drugs at levels that necessitate charitable intervention. It merely institutionalizes corporate negligence under the guise of compassion. One must ask: if the market cannot sustainably provide essential medicines, why is it allowed to exist in this form?
Just wanted to say thanks for writing this. I was about to give up on my med until I found RxHope. Got approved in 8 days. My doc’s access specialist helped me fill out the forms. Seriously, if you’re reading this and you’re scared or overwhelmed-just start. Don’t wait till you’re out. One step at a time. You got this.
Also, if your insurance says the PAP doesn’t count toward your deductible, ask them for the policy in writing. They hate doing that. And then go to a nonprofit. They’ll help.
Biggest tip I can give: call your pharmacy. Not the mail order one. The local one. They know all the tricks. I had a guy at my CVS who helped me get a $0 copay for my drug. He knew which foundations had extra funds that month. He didn’t charge me anything. Just did it because he’s a good person.
Also, keep a folder. Paper or digital. Everything. Even the denial letters. You’ll need them later.
And if your doctor says ‘I don’t know’-ask for the social worker. They’re the real MVPs.
Wow. Another feel-good story about how broken the system is. Congratulations. You’ve turned a structural failure into a checklist. You didn’t fix anything. You just taught people how to beg better. This isn’t help. It’s damage control for corporate greed.
Wait so if I’m on Medicare I can’t get help from the drug company but I can from a nonprofit? So like I just need to find some random org that’s not tied to the pharma? How do I even find those? Is there a list? Someone please link me. I’m scared I’m gonna lose my med.
From India, I want to say this: your system is brutal but your people are strong. I’ve seen patients here fight for medicine too, but with less resources. You have RxHope, you have navigators, you have voices. Don’t underestimate that. Keep pushing. And if you ever come to India, I’ll buy you chai. We don’t have PAPs but we have community. You’re not alone.
It’s worth noting that accumulator adjustments are not merely a policy quirk-they represent a violation of the fiduciary duty insurers owe to policyholders. The practice effectively nullifies the economic benefit conferred by third-party assistance, thereby rendering the PAPs functionally inert for a significant subset of beneficiaries. This constitutes a form of financial coercion under the guise of cost containment.
Look, I’m not here to cry about it. I’m here to say this: if you’re applying for PAPs, you’re already losing. The system was designed to make you beg. The fact that you’re reading this means you’re still alive. But don’t celebrate the crumbs. Demand the whole damn table. These companies make billions. You’re not asking for charity-you’re asking for justice. And if you’re not mad right now, you’re not paying attention.