When you’ve had a transplant, your life depends on keeping your immune system in check. That’s where cyclosporine and tacrolimus come in. These drugs stop your body from rejecting the new organ. But here’s the problem: when your insurance forces you to switch from brand-name to a generic version, things can go wrong-fast.
Why These Drugs Are So Tricky
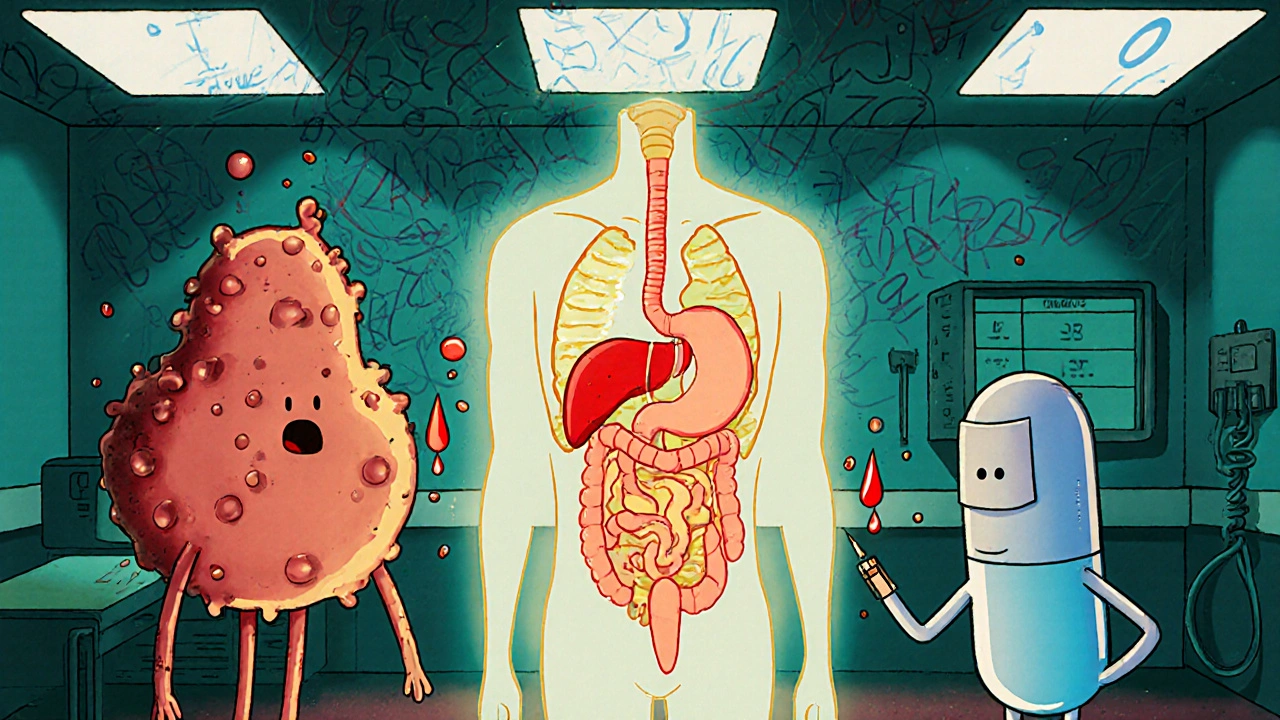
Cyclosporine and tacrolimus are both calcineurin inhibitors. They work the same way: they block T-cells from attacking your new kidney, liver, or heart. But that’s where the similarity ends. Tacrolimus works at 20 to 100 times lower doses than cyclosporine. A typical tacrolimus dose is 5 mg twice a day. Cyclosporine? Around 150 mg twice a day. The numbers look wildly different, but both are meant to hit the same therapeutic target. The real danger lies in their narrow therapeutic index. That means the difference between a dose that works and one that’s toxic is tiny. For tacrolimus, the safe blood level range is 5-15 ng/mL during the first few months after transplant. Go below 5, and your body might start rejecting the organ. Go above 15, and you risk kidney damage, seizures, or even death. Cyclosporine’s range is wider (100-200 ng/mL), but even then, small changes in absorption can cause big problems.Generic Versions Are Everywhere-But Not the Same
In 2025, over 92% of tacrolimus and cyclosporine prescriptions in the U.S. are generic. That’s a good thing for your wallet. Brand-name Prograf costs $1,200-$1,500 a month. Generic tacrolimus? Around $300-$500. Neoral, the brand-name cyclosporine, runs $800-$1,000. Generic versions drop that to $150-$300. But here’s what most people don’t know: not all generics are created equal. There are 14 FDA-approved generic tacrolimus products from 8 different manufacturers. For cyclosporine, there are 11 versions from 7 companies. Each uses different inactive ingredients-fillers, binders, oils-that affect how the drug is absorbed. Cyclosporine’s original formulation was oil-based and absorbed unpredictably. The newer microemulsion version (Neoral) fixed that. But some generics still use old formulations. A 2023 study found that only 41.7% of generic manufacturers provide detailed bioequivalence data to doctors. That means your pharmacist might switch you from one generic to another without telling you-and your drug levels could drop or spike overnight.Real People, Real Consequences
On Reddit’s r/transplant community, users share horror stories. One person switched from brand Prograf to a generic tacrolimus and saw their blood levels plunge from 8.5 to 5.2 ng/mL in two weeks. They ended up hospitalized with mild rejection. Another user said their nephrologist refused to let them try a different generic cyclosporine because their levels had been “all over the place” with the first one. A 2022 survey of 1,247 transplant patients found that 42.7% noticed new or worse side effects after switching to generic immunosuppressants. Nearly 1 in 5 needed a dose change because their levels became unstable. Meanwhile, medication non-adherence is 15.3% higher among people taking generics-not because they’re careless, but because they’re scared. They’ve seen what happens when the numbers don’t add up.
What Happens When You Switch?
Transplant centers know this risk. Most now have strict rules: if you switch from one generic to another-even if both are “FDA-approved”-you get weekly blood tests for at least four weeks. Some require daily checks for the first week. The American College of Clinical Pharmacy recommends monitoring for 4-6 weeks after any switch. Why? Because absorption can change. One patient switched from a generic made by Mylan to one from Teva and saw their tacrolimus levels drop 30% within days. Another switched from one cyclosporine brand to another and developed tremors and high blood pressure-signs of toxicity. It’s not just about the drug. Timing matters. Taking your pill 30 minutes before or after your usual time can throw off absorption. Grapefruit juice? Avoid it. It blocks the enzyme (CYP3A4) that breaks down both drugs, causing levels to spike. Alcohol, certain antibiotics, and even some herbal supplements can interfere too.Doctors Are Fighting Back
Many transplant teams now use a “single generic source” policy. That means the pharmacy only stocks one brand of generic tacrolimus and one brand of generic cyclosporine. If you’re on one, you stay on it. No switching unless absolutely necessary. In 2023, 67.4% of major transplant centers adopted this approach. It’s not perfect-but it’s safer. Some hospitals even require patients to sign a form acknowledging they understand the risks of switching generics. Insurance companies hate it. It costs more to stock one brand instead of five. But for patients, it’s life-saving.
The New Hope: Extended-Release and Genetic Dosing
There’s some good news. In late 2023, Astellas got FDA approval for a new extended-release version of tacrolimus called LCP-tacrolimus. It’s designed to release the drug slowly, keeping levels steady all day. That means fewer peaks and valleys-less risk of rejection or toxicity. It’s not generic yet, but it’s a step toward more stable dosing. Even better? Pharmacogenetic testing. About 15-20% of people have a genetic variant (CYP3A5*1) that makes them metabolize tacrolimus way faster. These patients need much higher doses. A 2023 study in JAMA Internal Medicine showed that testing for this gene before starting tacrolimus cut the time to reach stable levels by 63%. That means fewer hospital visits, fewer dose changes, and less stress.What You Can Do
If you’re on a generic immunosuppressant, here’s what you need to know:- Stick with the same generic brand. Don’t let your pharmacy switch it without telling you.
- Take your pill at the same time every day-within one hour, no exceptions.
- Avoid grapefruit, pomelo, and Seville oranges. They’re dangerous with these drugs.
- Keep a log of your blood levels and any new symptoms: tremors, headaches, nausea, swelling, or unusual fatigue.
- Ask your transplant team: “Which generic brand am I on? Can we lock it in?”
- If you’re switched without warning, demand weekly blood tests for at least a month.
Is It Worth the Risk?
Yes, generics save money. Billions of dollars, in fact. But with drugs this powerful, the cost of a mistake isn’t just financial-it’s life or death. The European Medicines Agency and the International Transplant Society both warn: switching between generic versions of tacrolimus or cyclosporine without close monitoring can cause rejection or toxicity. That’s not a rumor. It’s science. It’s data. It’s real patient stories. You don’t have to choose between affordability and safety. You just need to be informed. Ask questions. Demand consistency. Track your numbers. Your new organ depends on it.Can I switch between different generic versions of tacrolimus or cyclosporine?
No-not without close medical supervision. Even though all generics are FDA-approved, they can have different absorption rates. Switching between brands can cause your blood levels to drop too low (risking rejection) or spike too high (causing toxicity). Most transplant centers require weekly blood tests for four to six weeks after any switch.
Why is tacrolimus preferred over cyclosporine?
Tacrolimus is more effective at preventing acute rejection. Studies show rejection rates are nearly half with tacrolimus compared to cyclosporine in the first year after transplant. It also leads to better long-term kidney function. However, it carries a higher risk of post-transplant diabetes and neurological side effects like tremors. For most patients, the benefits outweigh the risks.
How do I know if my generic immunosuppressant is working?
You need regular blood tests to check your drug levels. For tacrolimus, levels should stay between 5-15 ng/mL in the first few months. For cyclosporine, aim for 100-200 ng/mL. If your levels suddenly change after a switch, or if you feel worse (headaches, nausea, swelling, fatigue), contact your transplant team immediately. Don’t wait.
Are there any foods or supplements I should avoid?
Yes. Grapefruit, pomelo, and Seville oranges block the enzyme that breaks down both drugs, causing dangerous spikes in blood levels. Avoid them completely. Also avoid St. John’s wort, echinacea, and high-dose vitamin E-they can lower drug levels. Always check with your pharmacist before starting any new supplement.
What should I do if my insurance forces me to switch to a different generic?
Insist on a plan. Ask your transplant team to request a prior authorization for your current generic. If that fails, demand weekly blood tests for at least four weeks after the switch. Keep a log of your levels and symptoms. If your levels become unstable, your doctor can appeal to your insurer for a medical exception to stay on your original brand.
Is there a way to avoid generic switching altogether?
Some transplant centers use a “single generic source” policy, meaning they only stock one brand of each drug. Ask if your center does this. You can also ask your doctor to write a letter of medical necessity explaining why consistency matters. Many insurers will approve a brand-name or specific generic if you can prove switching puts your transplant at risk.
Can genetic testing help with dosing?
Yes. About 1 in 5 people have a gene variant (CYP3A5*1) that makes them break down tacrolimus faster. These patients need much higher doses. Testing for this gene before starting the drug can cut the time to reach stable levels by over 60%, reducing the risk of rejection or toxicity. Ask your transplant team if genetic testing is available.
Just got switched to a new generic tacrolimus last month. My levels dropped from 8.1 to 4.9 in 10 days. No warning. No notice. Just a new bottle at the pharmacy. I called my transplant center immediately - they freaked out. Now I’m on weekly labs for the next month. If you’re on one of these, don’t let them switch you without a fight. I’m lucky I caught it.
Oh, so now the FDA is just a puppet of Big Pharma and Big Insurance? Of course they approve 14 different generics with zero standardized absorption data - because they don’t want you to know that the same pill from two different companies can kill you or make your new kidney explode. They’re letting pharmacists play Russian roulette with your life. And the worst part? They’ll tell you it’s ‘bioequivalent’ while your bloodwork screams otherwise. Wake up, people. This isn’t medicine - it’s corporate negligence dressed in lab coats.
Hi everyone, I’m from India and my brother had a kidney transplant 3 years ago. He’s on generic tacrolimus - same brand since day one. We learned the hard way: never switch. In our country, generics are cheaper but often inconsistent. We found a pharmacy that stocks only one brand and we stick with it. Also, avoid turmeric supplements - they interfere with absorption. I know it sounds weird, but trust me, it’s real. Your organ doesn’t care about cost - it just wants stable levels. Stay consistent, stay safe. 🙏
As someone who’s been on tacrolimus for 8 years, I can’t stress this enough: know your brand. Write it down. Take a picture of the bottle. Ask your pharmacist every single time you refill - ‘Is this the same one?’ If they say ‘Oh, it’s just another generic,’ walk out. Your life isn’t a cost-saving experiment. Also, grapefruit juice? No. Just no. Even one glass can send your levels through the roof. I’ve seen too many people get hospitalized over this. You’re not being paranoid - you’re being smart.
So… are we seriously supposed to believe that the FDA doesn’t know these generics aren’t interchangeable? C’mon. They’ve known for years. They just don’t care because they get kickbacks from Big Pharma. And don’t even get me started on how insurance companies force switches on people who can’t afford the brand. It’s not a mistake - it’s a massacre. I’ve got a friend who lost her liver transplant because they switched her to a cheap cyclosporine. The paperwork? ‘Bioequivalent.’ The result? Dead. This isn’t healthcare. It’s euthanasia by spreadsheet.
i just wanna say thank you for writing this. i’ve been on cyclosporine since 2021 and i never knew how dangerous switching generics could be. i thought all generics were the same. i’ve been taking mine at 7pm every night and i avoid grapefruit like the plague. i didn’t even know about the gene test thing - gonna ask my doc next week. i feel less alone now. thanks for the info. you’re a lifesaver.
Bro, I’m on tacrolimus too! My levels are stable since I stuck with one generic - Teva. I even made a note in my phone: 'DO NOT SWITCH.' 😅 Also, I take it with a small snack - not empty stomach. My nurse told me that helps absorption. And yeah, grapefruit? I don’t even smell it anymore lol. Stay strong, fam. You got this! 💪
Wait… so you’re telling me the government is letting drug companies change the fillers in my life-saving medicine without telling me? And they call this ‘science’? I bet they’re also hiding that the pills are laced with microchips to track transplant patients. I’ve been getting weird headaches since my last refill… it’s not the drug - it’s the tracking. They want to know when we’re dying so they can sell our organs faster. I’m switching to herbal tea. At least that’s not monitored.
Stick to one brand. Test weekly after any switch. Avoid grapefruit. Ask about genetic testing. That’s it. Simple. No drama. No conspiracy. Just facts. Your transplant is worth the effort. Don’t let a pharmacy save $50 on your life. You’re not just a patient - you’re a survivor. Keep going.