When your doctor prescribes a brand-name medication but your insurance says you must switch to the generic version - and you know it won’t work for you - you’re not alone. Thousands of people face this every year. Insurance companies push generics to save money, but sometimes, the generic just doesn’t do the job. It might cause side effects, fail to control your condition, or interact badly with other meds you’re taking. If that’s you, you have rights. You can appeal. And more often than not, you win - if you do it right.
Understand Why Your Insurance Denied the Brand-Name Drug
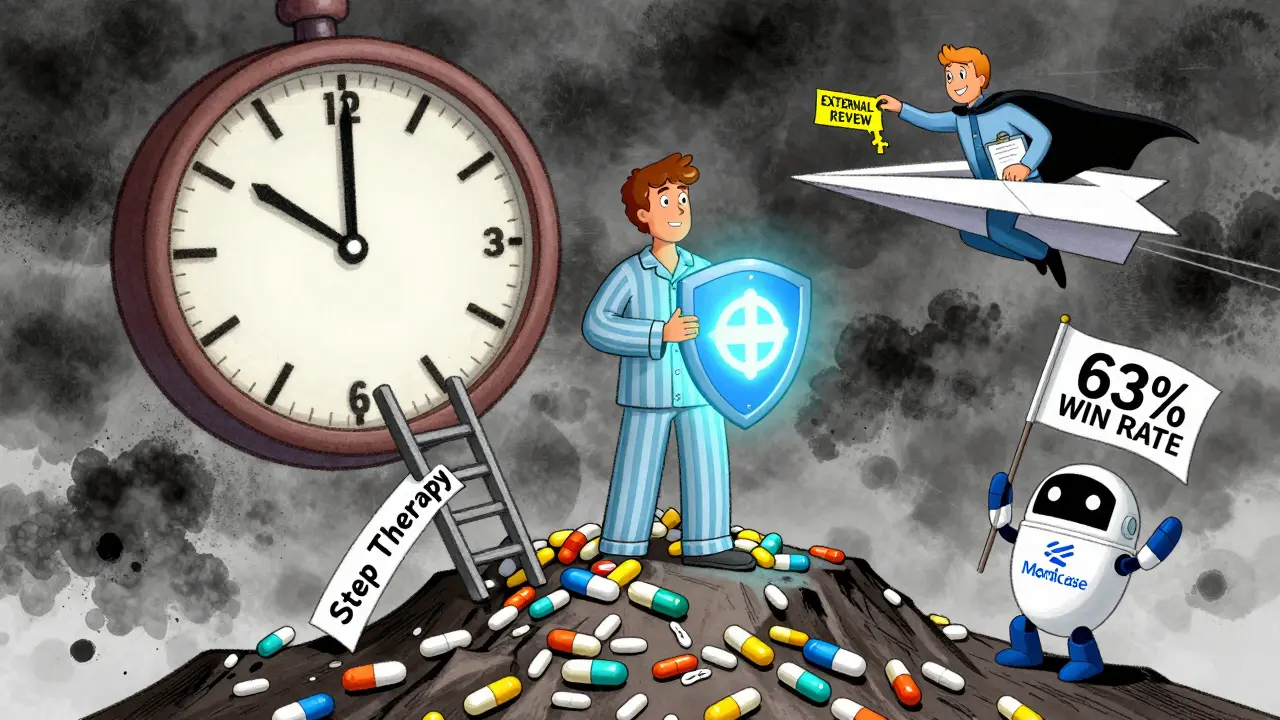
Your insurance plan has a list of approved drugs called a formulary. Generics are usually on the bottom tier because they’re cheaper. Brand-name drugs? They’re often blocked unless you prove you absolutely need them. This is called step therapy: you must try the cheaper option first, even if your doctor says it won’t work.
When you get denied, your Explanation of Benefits (EOB) letter should explain why. Look for phrases like:
- “Generic equivalent available”
- “Step therapy requirement not met”
- “Prior authorization denied”
Don’t ignore this letter. It contains your appeal deadline - usually 180 days from the denial date for private insurance. Medicare gives you only 120 days. Miss it, and you lose your chance.
Gather the Right Documentation
Insurance companies don’t care what you think. They care what your doctor says - and only if it’s written down clearly. The single biggest reason appeals fail? Poor documentation.
Your doctor needs to write a letter of medical necessity. This isn’t a quick note. It must include:
- Why the generic won’t work for you (e.g., “Patient experienced severe nausea and dizziness with generic metformin; brand-name Glucophage controlled symptoms effectively for 18 months”)
- Proof you’ve already tried alternatives (e.g., “Patient tried three different generic SSRIs over 14 months, all resulted in suicidal ideation”)
- References to clinical guidelines (e.g., “Per American Diabetes Association 2023 Standards of Care, individualized therapy is recommended when prior agents cause adverse reactions”)
According to a GoodRx analysis of 15,000 appeals, 78% of successful cases included this kind of detailed clinical reasoning. Only 29% of failed appeals did.
Also collect:
- Pharmacy records showing prior failed attempts
- Lab results or doctor’s notes documenting adverse reactions
- Your prescription history
The Crohn’s & Colitis Foundation found that 83% of successful appeals had at least two documented failed alternatives. More is better.
Submit the Formal Appeal
Don’t call. Don’t email. Fill out the official form.
Most insurers have a Prescription Drug Prior Authorization or Step Therapy Exception Request Form. You can usually download it from your plan’s website or request it by phone. If you can’t find it, call customer service and ask for “the form to appeal a generic substitution denial.” Write down the rep’s name and ID.
Complete every section:
- Your full name, date of birth, insurance ID
- Exact drug name and dosage you’re requesting
- Reason for denial (copy from your EOB)
- Attach the doctor’s letter and supporting documents
Send it certified mail with return receipt. Or submit it online if your insurer offers it. Keep copies of everything. This isn’t optional - it’s your paper trail.
Request a Peer-to-Peer Review
This is where most appeals turn around.
After you submit your paperwork, the insurance company’s medical team will review it. But here’s the secret: if your doctor asks for a peer-to-peer review, they can speak directly to the insurer’s doctor. No middleman. No form. Just two professionals talking.
Studies show peer-to-peer reviews succeed over 75% of the time when the prescribing doctor is prepared. Your doctor should say something like:
“I’m requesting a peer-to-peer review with your medical director. My patient has tried three generics for type 2 diabetes and developed severe hypoglycemia each time. Semaglutide is the only option that stabilized their glucose without side effects. Per ADA guidelines, this is a medically necessary exception.”
Many insurers will schedule this within 24-48 hours. Don’t let your doctor skip this step.

Know Your Timelines
Insurance companies have deadlines - and you should too.
- Standard appeal: 30 days for new prescriptions, 60 days for ongoing ones
- Expedited appeal (urgent case): 4 business days if you’re at risk of serious harm (e.g., uncontrolled seizures, diabetic ketoacidosis, suicidal depression)
- Medicare Part D: 7 days for standard, 72 hours for urgent
If you don’t hear back in time, follow up. Call every 3-5 days. Ask: “Has my appeal been reviewed? Can I get a case number?” Keep a log of every call: date, time, name, what was said.
One patient in a T1D Exchange case study waited 52 days for approval after three denials. She called every week. On day 53, she got the green light - because she never gave up.
What If Your Appeal Gets Denied Again?
Most plans offer a second level of appeal. Don’t stop here.
For commercial insurance, you can request an external review by an independent third party. This is your last internal shot. For Medicare, you move to Level 2: Independent Review Entity. This is where the odds get better. CMS data shows 63.2% of appeals get overturned at this stage.
At this point, you may need help. Contact your state’s Department of Insurance. In California, they resolve 92% of formal complaints. In New York, they require insurers to respond within 72 hours for peer reviews. Even if you’re not in those states, your insurance commissioner can still intervene.
Use this free resource: call your state’s insurance helpline. They’ll walk you through the next steps. No charge. No lawyer needed.
Common Mistakes That Kill Your Appeal
Here’s what most people do wrong:
- Waiting too long to start - deadlines are strict
- Asking the pharmacist to help - they can’t write medical letters
- Using vague language: “The generic doesn’t work” instead of “Patient had three episodes of hypoglycemic coma on generic metformin”
- Not including the doctor’s license number or contact info on the letter
- Forgetting to send the form - some people only send the letter
Johns Hopkins found that 41% of failed urgent appeals were because the request wasn’t labeled correctly as “urgent.” If your condition could land you in the ER, mark it as urgent - and explain why.
Success Stories: What Works
One woman with rheumatoid arthritis was denied Humira because her plan required trying two generics first. She’d tried both - both caused severe skin reactions. Her doctor’s letter cited the American College of Rheumatology guidelines on biologic therapy. She submitted the appeal with lab results showing elevated CRP levels. Approved in 11 days.
A man with Type 1 diabetes was denied semaglutide because his insurer said insulin was “sufficient.” His doctor showed 14 months of blood sugar logs - all over 200 mg/dL. He had two hospitalizations for DKA. The appeal was approved after a peer-to-peer call. He’s now stable.
These aren’t rare. In 2022, 72.3% of denied generic appeals were overturned. That’s more than 7 out of 10 people who fought back.
When to Get a Patient Advocate
If you’re overwhelmed, tired, or dealing with a chronic illness, you don’t have to do this alone.
Organizations like the Patient Advocate Foundation offer free help. They’ll review your documents, call your insurer for you, and even draft letters. Their clients have a 65% success rate - compared to 32% for people who go it alone.
They’re not lawyers. They’re trained advocates who know the system. And they work for you - not the insurance company.
Final Thought: This Is Your Right
Insurance isn’t your doctor. They don’t know your body. They don’t know your history. They’re not there to make you better - they’re there to manage costs. But the law says they can’t deny you care just because it’s expensive.
When you appeal, you’re not fighting the system. You’re using the system the way it was meant to be used. And if you do it right, you’ll get what you need.
Start today. Get your doctor’s letter. Fill out the form. Send it certified. Call every week. Don’t wait. Your health is worth it.
What if my doctor won’t help me with the appeal?
If your doctor refuses, ask why. Many don’t realize how simple the process is - or they’re overwhelmed. Try asking again, or ask for a nurse practitioner or physician assistant in the office. If that doesn’t work, contact your state’s medical society. They often have templates and can even call the insurer on your behalf. Some patient advocacy groups also provide pre-written letter templates doctors can sign.
Can I appeal if I’m on Medicare Part D?
Yes. Medicare Part D has a five-step appeal process. Start with a Coverage Determination Request (Form CMS-10463), signed by your doctor. If denied, you can escalate to an Independent Review Entity, which overturns 63% of cases. You have 60 days to file each level. Don’t wait - deadlines are strict. The Medicare Rights Center offers free phone counseling at 1-800-MEDICARE.
How long does an appeal usually take?
Standard appeals take 30 to 60 days. Urgent cases must be decided in 4 business days. If you’re on Medicare, standard reviews take 7 days, urgent ones 72 hours. Most people get a decision within 2-4 weeks if all paperwork is complete. Delays usually happen when documents are missing or the doctor’s letter is too vague.
Are there any free tools or templates to help?
Yes. The Patient Advocate Foundation offers free appeal letter templates for common conditions like diabetes, asthma, and autoimmune diseases. The Crohn’s & Colitis Foundation has downloadable forms for step therapy appeals. GoodRx also provides a step-by-step checklist. All are available online at no cost. Use them - they’re designed by people who’ve been through this.
Will my insurance raise my rates if I appeal?
No. Federal law prohibits insurers from penalizing you for filing an appeal. Your premiums, coverage, or access to care cannot be affected by exercising your rights. If someone tells you otherwise, report them to your state’s insurance commissioner. This is not just policy - it’s the law.
What if I need the medication right away?
Ask your doctor for a 30-day emergency supply. Many insurers allow this while your appeal is pending - especially if you’re at risk of hospitalization. Some pharmacies will also provide a short-term supply through patient assistance programs. Don’t go without. Fight for a bridge while you fight the system.

im trying to appeal my insulin right now and this guide is actually super helpful thanks!!
My doctor refused to write the letter so I used the Patient Advocate Foundation template-signed it myself and got approved in 17 days. They don’t need to sign it if you’re clear about your history. Just make sure the pharmacy records are attached.
Man, I wish I’d known about peer-to-peer reviews when I was fighting for my biologic. My doc just sent the form and assumed that was it. Turns out, the insurance doctor was a total jerk-until my doctor called him directly. Two days later, approval. The system’s broken, but the human connection? That still works. Don’t let your doctor skip that step. It’s the secret weapon.
From India here-our system is wild, but I’ve seen this play out with my cousin’s dad. Insurance here says ‘generic same’ but the generic made him dizzy for weeks. Took 4 months, 3 letters, and a call from his neurologist to the insurer’s medical director. They finally approved. The key? Documentation. Not yelling. Not begging. Just facts, dates, and clinical logic. You got this.
There is something profoundly unjust, yet profoundly human, about being forced to prove your body’s betrayal to a faceless algorithm. Insurance companies reduce suffering to a form field, yet the very act of appealing-of gathering lab results, of begging your doctor to write that letter-is an act of radical self-advocacy. You are not asking for a favor. You are asserting your right to be treated as a person, not a cost center. And when you win? You don’t just get your medication. You reclaim your dignity.
This is all propaganda. The generics are just as good. Your doctor is probably being paid by Big Pharma to push brand names. I’ve been on generics for 12 years-no issues. People who can’t tolerate generics are either hypochondriacs or addicts. And peer-to-peer reviews? That’s just doctors protecting each other’s paychecks. The system works fine. You just don’t like being told no.
My sister got denied for her epilepsy med and the insurance company said ‘try generic’-she had a seizure in the ER because of it. Then they sent her a letter saying ‘we reviewed your case and determined your condition is not severe enough to warrant brand-name.’ SEVERE ENOUGH?? She almost DIED. Now they’re being sued. Don’t just appeal-start a TikTok. People need to see this.
Wow. So if you’re rich enough to afford brand-name meds, you get to play the system. But if you’re poor and on Medicaid? Tough luck. This whole guide is just a fancy way of saying ‘if you have time, energy, and a doctor who cares, you win.’ Everyone else? Suffer silently. And hey, congrats on your 72% success rate-guess that means 28% of people just gave up and died. Classic.
Did you know that 90% of these ‘appeals’ are approved because the insurance companies are secretly paid by drug manufacturers to approve them? It’s a scam. The ‘formulary’? A front. The ‘peer review’? A puppet show. They want you to think you’re fighting the system-but you’re just a pawn in their profit game. Your doctor’s letter? Probably already been edited by their legal team. Don’t trust any of this.
I had to appeal for my son’s ADHD med. The first letter from my doctor was too vague-just said ‘generic doesn’t work.’ Got denied. We redid it with exact dosages, side effect logs, school performance reports, and a reference to the AACAP guidelines. Approved on the second try. The difference? Specifics. Not emotion. Not yelling. Just cold, clear, documented facts. It’s boring, but it works.
This is one of the most well-researched, compassionate, and actionable pieces I’ve read on this topic in years. The emphasis on peer-to-peer reviews is spot-on-it’s the single most underutilized lever in the entire system. And the warning about labeling appeals as ‘urgent’? Critical. So many people miss that. Thank you for not just informing, but empowering.
Let me tell you something about capitalism: it turns health into a commodity, and you, the patient, into a number on a spreadsheet. This guide? It’s not a guide-it’s a survival manual. And the fact that you have to fight so hard just to breathe? That’s not a flaw in the system. That’s the system working exactly as intended. So yes-appeal. But don’t forget: the real battle isn’t with the insurer. It’s with the ideology that says your life has a price tag.
I spent 8 months on this. Got denied 4 times. My doctor was too busy. So I wrote the letter myself-used the template from Crohn’s & Colitis Foundation, filled in my history, printed it, got it notarized, and sent it certified. Then I called every single day. On day 247, they called me back and said, ‘We’re approving it.’ I cried. Not because I got the drug. Because I proved I wouldn’t be erased.
Just submitted my appeal today. Used the GoodRx checklist. Doctor’s letter is done. Sent it certified. Waiting now. Fingers crossed. This system is exhausting-but I’m not giving up. If you’re reading this and you’re in the middle of it? You’re not alone. Keep going. One step at a time.