For most people, the idea of a new generic drug being approved without testing it on humans sounds impossible. But it’s not science fiction-it’s standard practice for certain drugs, thanks to something called a bioequivalence waiver. The U.S. Food and Drug Administration (FDA) lets drugmakers skip expensive, time-consuming human trials if they can prove through lab tests that their version of a drug behaves the same way in the body as the brand-name version. This isn’t a loophole. It’s a science-backed shortcut that saves millions and gets life-saving medicines to patients faster.
What Exactly Is a Bioequivalence Waiver?
A bioequivalence waiver, or biowaiver, is when the FDA says: "You don’t need to give this drug to volunteers to prove it works the same." Instead, you can use lab tests-specifically, dissolution testing-to show that your generic drug releases its active ingredient at the same rate and in the same amount as the original. This applies only to immediate-release solid oral tablets and capsules, not liquids, injections, or extended-release pills. The legal basis comes from 21 CFR 320.22 and 320.24(a). These rules say the FDA must accept the most accurate, sensitive, and reproducible method to prove bioequivalence. For some drugs, that’s not a blood test in humans-it’s dissolving the pill in lab solutions that mimic stomach and intestinal fluids.How Does the FDA Decide Which Drugs Qualify?
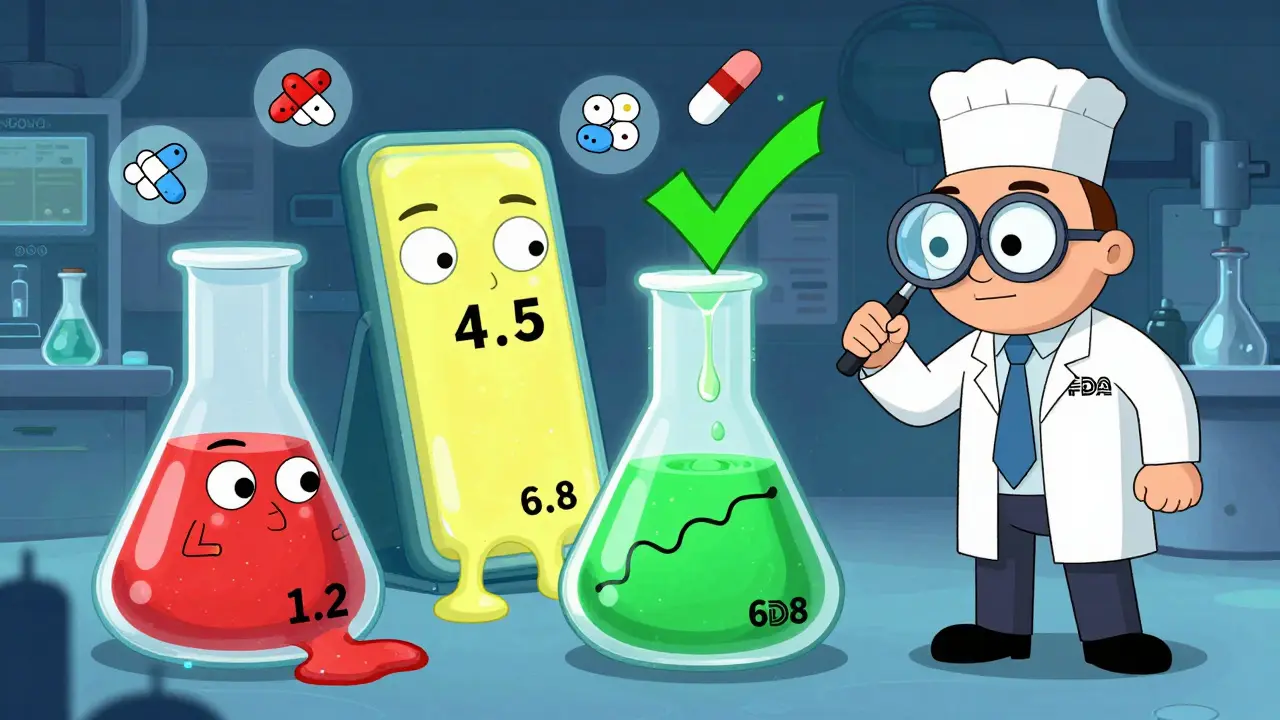
The key is the Biopharmaceutics Classification System (BCS). It groups drugs based on two things: how well they dissolve in water (solubility) and how easily they cross into the bloodstream (permeability). Only two classes qualify for waivers:- BCS Class I: High solubility, high permeability. These are the easiest to waive. Examples include metformin, atenolol, and ciprofloxacin.
- BCS Class III: High solubility, low permeability. These are trickier. The FDA requires that the generic has the exact same inactive ingredients (excipients) and same proportions as the brand. Also, the drug must not be absorbed in a specific part of the gut-otherwise, differences in formulation could matter.
- The drug dissolves rapidly-85% or more in 30 minutes across pH 1.2, 4.5, and 6.8.
- The dissolution profiles of the generic and brand are nearly identical. The similarity factor (f2) must be 50 or higher.
- The drug is highly permeable-90% or more of the dose is absorbed in the body.
Why Does This Matter for Patients and Companies?
Skipping human studies saves a ton of time and money. A typical bioequivalence study costs between $250,000 and $500,000 and takes 6 to 12 months. For a company making dozens of generics, that adds up fast. One formulation scientist reported saving $4.2 million over three years by using waivers for 12 products. That money goes into more research, lower prices, or both. Patients benefit too. In 2022, biowaivers helped speed up generic approvals by an average of 7.3 months per drug. That means cheaper versions of drugs like lisinopril or levothyroxine hit the market faster. According to IQVIA, this has added $1.2 billion in annual savings to the U.S. healthcare system.
What Happens If You Don’t Meet the Criteria?
Most biowaiver applications get rejected for one of three reasons:- Poor dissolution method: The test doesn’t catch differences between formulations. FDA found 35% of rejections were due to this.
- Wrong pH conditions: Dissolution tests must use pH 1.2 (stomach), 4.5 (upper intestine), and 6.8 (lower intestine). If you use only one pH, you’re likely to fail.
- Missing data: You need at least 12 tablets per batch tested at six time points: 10, 15, 20, 30, 45, and 60 minutes.
Who’s Using This the Most?
Large generic drugmakers like Teva and Mylan use biowaivers in 25-30% of their development pipelines. Smaller companies use them less-only 10-15%-because developing the right dissolution methods requires expertise and time. It takes 2-3 months just to validate a dissolution test, plus another 1-2 months to compare products. The FDA encourages early communication. Companies that request a Pre-ANDA meeting with the agency have a 22% higher approval rate for biowaivers. That’s not luck-it’s strategy. The FDA’s Office of Generic Drugs reviews these requests and gives feedback before companies spend hundreds of thousands on testing.What’s Changing in 2025?
The FDA is quietly expanding the scope of biowaivers. In 2022, they released a draft guidance to allow waivers for more BCS Class III drugs, as long as additional data is provided. In 2023, they launched a pilot program to test whether certain narrow therapeutic index drugs-like warfarin or levothyroxine-could qualify under stricter rules. Their 2023-2027 strategic plan says they want to increase biowaiver approvals by 25% over the next few years. That means more refined models, better in vitro-in vivo correlations, and possibly new categories. But there’s a catch: 85% of complex products-like delayed-release or chewable tablets-still can’t use waivers. The science isn’t there yet.
Is This Safe?
Yes. Over 95% of the time, BCS Class I biowaivers correctly predict whether a generic will perform like the brand in the body. That’s based on data from the American Association of Pharmaceutical Scientists (AAPS), which tracked real-world outcomes over years. The FDA’s own data shows that between 2012 and 2016, 78% of complete biowaiver applications were approved. There’s no evidence that drugs approved via biowaiver are less effective or cause more side effects. The system works because it’s built on decades of pharmacokinetic research. It’s not about cutting corners-it’s about using better science.What About Other Countries?
The U.S. isn’t alone. The International Council for Harmonisation (ICH) published M9 guidance in 2021, which standardizes BCS-based biowaivers across the U.S., EU, Japan, Canada, and other major markets. This means a company can use the same data to get approval in multiple countries, making global generic development faster and cheaper.Final Thoughts
Bioequivalence waivers aren’t a loophole. They’re a smart, science-driven way to avoid unnecessary human testing when the data already proves a drug will work the same. For generics, it’s a lifeline. For patients, it’s faster access to affordable medicine. For regulators, it’s a way to focus resources where they’re truly needed. The key is rigor. If you’re not meeting the dissolution criteria, if you’re skipping pH testing, or if you’re guessing about permeability-you’ll get rejected. But if you’ve done the work, the FDA will trust your data. And that’s how science should work.Can any generic drug get a bioequivalence waiver?
No. Only immediate-release solid oral dosage forms (tablets and capsules) that meet specific BCS criteria can qualify. Modified-release, liquids, injectables, and topical products are not eligible. Narrow therapeutic index drugs are generally excluded, except under special FDA guidance.
What’s the difference between BCS Class I and Class III for waivers?
BCS Class I drugs (high solubility, high permeability) only need matching dissolution profiles to qualify. BCS Class III drugs (high solubility, low permeability) require identical excipients, same proportions, and proof that absorption isn’t location-dependent in the gut. Class III waivers are harder to get and have stricter requirements.
How accurate are dissolution tests compared to human studies?
For BCS Class I drugs, dissolution tests are more accurate than human studies in detecting formulation differences. Studies show over 95% concordance between in vitro results and actual in vivo performance. The FDA considers them the most sensitive and reproducible method for these drugs.
Why do some biowaiver applications get rejected?
Most rejections happen because the dissolution method isn’t discriminatory enough to detect differences between formulations. Other common reasons include testing at the wrong pH levels, using fewer than 12 tablets per batch, or failing to meet the f2 similarity factor of 50 or higher.
Do I need to do human studies if I apply for a waiver?
No-if your application is approved, you don’t need any human studies. But if the FDA rejects your waiver request, you’ll be required to submit an in vivo bioequivalence study. Many companies run both the dissolution test and a human study in parallel to avoid delays.
How long does it take to get a biowaiver approved?
Once submitted, FDA reviews biowaiver requests as part of the overall ANDA application. Approval timelines vary, but companies that request a Pre-ANDA meeting see approval rates 22% higher. On average, the entire process-from method development to approval-takes 12-18 months for well-prepared applications.
Man, I never realized how much science goes into generic drugs. I just thought they were cheaper copies, but this is like a whole different level of precision. Dissolution profiles and f2 factors? That’s next-level stuff. The FDA’s actually being smart here-not cutting corners, just using better tools.
It’s wild how much time and money this saves. I work in pharma logistics-seeing those 7-month time savings add up across dozens of drugs? It’s insane. Patients get meds faster, companies stay afloat, and the system doesn’t collapse. Science wins.
Let me guess-Big Pharma pushed this so they could keep their brand drugs expensive while letting generics flood the market with ‘identical’ pills that actually behave differently. They’re using ‘BCS Class I’ as a smokescreen. What if the dissolution test doesn’t catch absorption differences in people with IBS or liver damage? Who’s monitoring that? They don’t test on humans, so how do they know it’s safe for real bodies? This smells like corporate convenience disguised as science.
It’s funny how we fear what we don’t understand. We’re okay with pills dissolving in our stomachs, but when someone says ‘we don’t need to test on people’-instant panic. But if the science says the pill behaves the same in a simulated gut as it does in a human, why do we need to stick needles in volunteers? We’ve been doing this with food and chemicals for decades. The body isn’t magic-it’s chemistry. Trust the data, not the fear.
So you’re telling me they let companies skip human testing… but still charge $400 for a 30-day supply of lisinopril? Like, what’s the point? If it’s so cheap to make, why am I still broke? This isn’t science-it’s capitalism with a lab coat.
While the regulatory framework described is indeed grounded in rigorous scientific principles, one must also acknowledge the ethical imperative to ensure patient safety through empirical validation. The reliance on in vitro models, though statistically robust, should be continually re-evaluated in light of inter-individual pharmacokinetic variability. Transparency in dissolution methodology and public access to comparative data are paramount to maintaining public trust.
You Americans think you invented science. In Nigeria, we’ve been making generics for 30 years without your fancy pH buffers. We just test one tablet, swallow it, and see if the headache goes away. Your 12 tablets per batch? Your f2 factor? Your three pH levels? That’s overkill. If it looks the same and costs less, it works. Your system is bloated. We don’t need 18 months to approve a pill.
Really cool breakdown. I’m from India-we make a ton of generics here. What’s wild is how many small labs here try to cut corners on dissolution testing. They’ll use only pH 6.8 because it’s easier, and then wonder why the FDA rejects them. This post is basically a cheat sheet for anyone trying to play the game right. Thanks for the clarity.
Brilliantly articulated. The convergence of regulatory science, pharmacokinetic modeling, and global harmonization through ICH M9 represents a triumph of evidence-based policy. This is how medicine should evolve-efficient, ethical, and anchored in reproducible data.
i just read this and my brain hurt. like… why do they need 12 tablets? and why 6 time points? and why can’t they just test on like… 10 people? this is so complicated. also i think the FDA is secretly run by robots. someone please explain this to me in emojis?