Muscle Spasm Risk Assessment Tool
This tool helps you evaluate your risk factors for muscle spasms and suggests preventive measures.
Personal Information
Quick Takeaways
- A muscle spasm is an involuntary, sudden contraction triggered by nerve misfires.
- Calcium overload, low electrolytes, and dehydration are the top biochemical culprits.
- Spasms differ from harmless twitches: they’re painful, last longer, and often involve many fibers.
- Immediate relief comes from stretching, hydration, and restoring electrolytes.
- Seek medical help if spasms are frequent, severe, or accompanied by weakness.
Ever felt a sudden, painful knot in your calf after a night of poor sleep? That jolt is a muscle spasm, and while it feels mysterious, the body follows a clear chain of events. Below we’ll walk through each step, from the nerve signal that sparks the contraction to the biochemical cascade that locks the muscle in place. By the end, you’ll know why they happen, how to calm them down, and when a spasm is a sign you should see a doctor.
muscle spasm is a sudden, involuntary contraction of a muscle or group of muscles. It typically lasts from a few seconds to several minutes and can be intensely painful. The process starts in the nervous system, but the muscles themselves hold the final keys to pain and release.
1. The Nerve‑Muscle Conversation
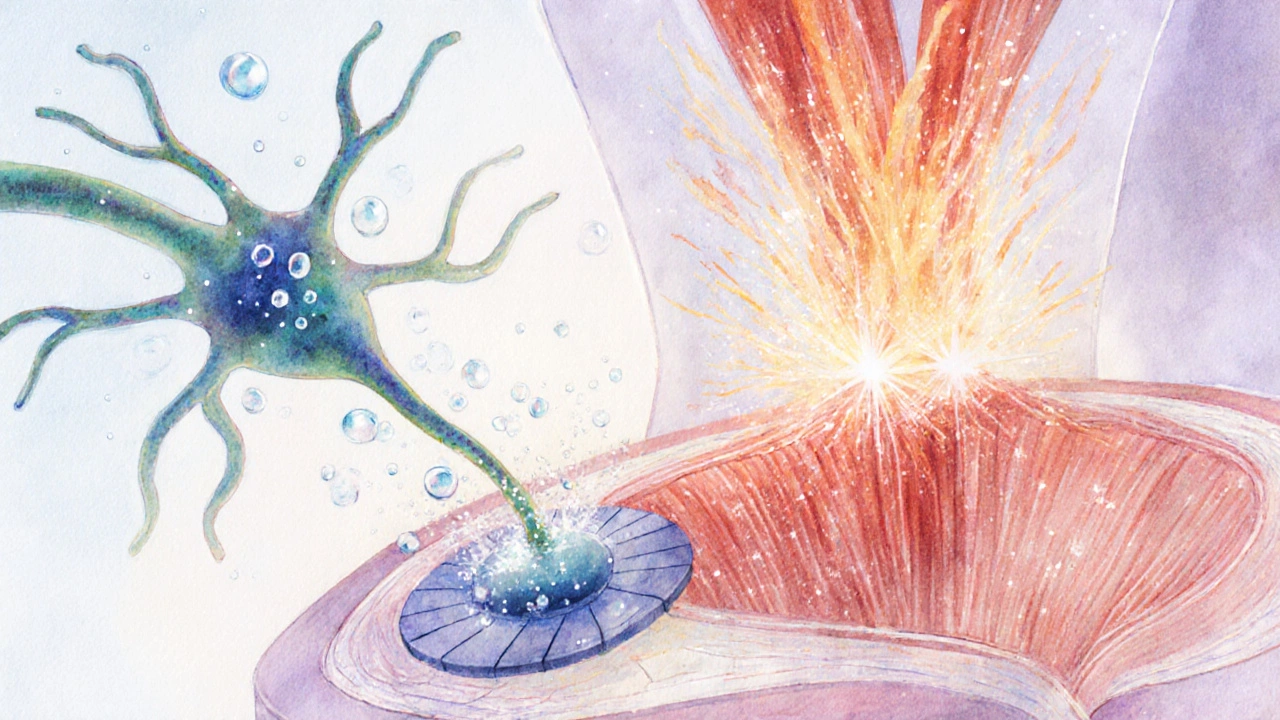
Every movement begins with a motor neuron a nerve cell that carries signals from the spinal cord to muscle fibers. When the brain decides to move, the motor neuron fires an electrical impulse called an action potential. This impulse travels down the axon and reaches the neuromuscular junction-the tiny gap where nerve meets muscle.
At the junction, the neuron releases acetylcholine a neurotransmitter that binds to receptors on the muscle cell membrane. The binding opens ion channels, allowing sodium ions to flood in, which depolarizes the muscle cell and triggers its own electrical signal.
2. Calcium Floods the Fibers
Once the muscle cell’s membrane is depolarized, the signal rushes into the interior via the transverse (T‑tubule) system, reaching the sarcoplasmic reticulum a specialized storage organelle that releases calcium ions into the muscle cytoplasm. The sarcoplasmic reticulum opens its calcium channels, dumping massive amounts of calcium ion the key messenger that initiates muscle contraction into the surrounding fluid.
Calcium binds to troponin, a protein that shifts tropomyosin out of the way on the actin filament. This exposure lets myosin heads grab onto actin, pulling the filaments past each other and shortening the muscle-i.e., a contraction.
3. Why the Muscle Won’t Let Go
In a normal contraction, calcium is quickly pumped back into the sarcoplasmic reticulum by the ATP‑driven calcium‑ATPase pump. The removal of calcium lets troponin revert, tropomyosin covers the binding sites again, and the muscle relaxes.
During a spasm, the pump falters or calcium influx overshoots. Common reasons include:
- Electrolyte imbalance: Low levels of potassium, magnesium, or sodium disrupt the pump’s efficiency.
- Dehydration: Less water means fewer ions in the extracellular fluid, raising the threshold for proper repolarization.
- Muscle fatigue: Exhausted fibers accumulate metabolic by‑products like lactic acid, which interfere with calcium handling.
- Excessive nerve firing: Hyperactive motor neurons keep releasing acetylcholine, sustaining the calcium surge.
When calcium stays high, the actin‑myosin cross‑bridges keep gripping, locking the muscle in a painful state.
4. Types of Involuntary Muscle Contractions
| Type | Typical Duration | Pain Level | Primary Cause |
|---|---|---|---|
| Muscle cramp (spasm) | seconds‑minutes | moderate‑severe | Electrolyte shortage, dehydration, fatigue |
| Fasciculation (twitch) | milliseconds‑seconds | usually none | Spontaneous motor‑neuron discharge |
| Tetany (continuous contraction) | minutes‑hours | severe | Severe hypocalcemia, nerve disorders |
Understanding the differences helps you decide if a simple stretch will work or if you need professional care.
5. Quick Relief Strategies You Can Try Now
When a spasm hits, the goal is to reverse the calcium overload and relax the cross‑bridge cycle. Here are five evidence‑backed tricks:
- Stretch the muscle gently: Lengthening the fiber pulls the attached tendons, sending a signal to the spinal cord that the muscle should relax.
- Apply heat for chronic cramps (increases blood flow) or cold for acute pain (reduces nerve firing).
- Hydrate with an electrolyte‑rich drink-think sports drink, coconut water, or a pinch of sea salt in water.
- Massage the trigger point: Gentle pressure improves local circulation and helps the calcium‑ATPase pump clear excess ions.
- Supplement if needed: Magnesium (300‑400mg) and potassium (2‑3g) are the most common defenders against recurrent cramps.
6. When a Spasm Signals a Bigger Issue
Most spasms are harmless, but certain patterns suggest underlying conditions:
- Frequent nighttime leg cramps that disrupt sleep.
- Spasms accompanied by swelling, redness, or a lump-possible muscle strain or compartment syndrome.
- Weakness after a spasm, indicating nerve compression (e.g., sciatica).
- Spasms that persist despite proper hydration and electrolytes-could be a metabolic disorder like hyperparathyroidism.
If any of these appear, schedule a visit with a physiotherapist or physician. Blood tests can check electrolyte levels, while EMG (electromyography) assesses nerve‑muscle communication.
7. Preventing Future Spasms
Prevention is easier than treating a full‑blown cramp. Incorporate these habits into your routine:
- Stay consistently hydrated-aim for at least 2L of fluid daily, more if you sweat heavily.
- Balance your diet with potassium‑rich foods (bananas, sweet potatoes) and magnesium sources (nuts, leafy greens).
- Warm up before intense activity; a 5‑minute dynamic stretch prepares the calcium pumps.
- Include regular low‑intensity stretching or yoga to keep muscles supple.
- If you’re on diuretics or certain blood‑pressure meds, ask your doctor about electrolyte monitoring.
By keeping the neural and chemical environment stable, you reduce the chance of those sudden, painful knots.
Frequently Asked Questions
Why do I get cramps at night but not during the day?
Overnight muscles are often less active, which can allow calcium to build up in the sarcoplasmic reticulum. Low ambient temperature and reduced fluid intake before bed also lower electrolyte levels, making nighttime cramps common.
Can stress cause muscle spasms?
Yes. Stress triggers the sympathetic nervous system, increasing motor‑neuron firing rates. The heightened neural activity can lead to excess acetylcholine release, which may provoke spasms, especially in already fatigued muscles.
Are muscle spasms the same as muscle strains?
No. A spasm is a functional, involuntary contraction, while a strain is a structural injury to muscle fibers or tendons caused by overstretching or overload.
Should I take painkillers for a cramp?
Over‑the‑counter NSAIDs can help with the pain but won’t address the underlying calcium overload. Combine medication with stretching and electrolyte restoration for faster relief.
When is it time to see a doctor?
If spasms occur more than three times a week, are accompanied by weakness, swelling, or last longer than 10 minutes, or you have a known medical condition (e.g., diabetes, kidney disease), schedule a medical evaluation.
Understanding the chain of events-from the motor neuron firing to calcium’s stubborn stay-gives you concrete ways to stop a spasm in its tracks. Keep an eye on hydration, electrolytes, and muscle conditioning, and you’ll spend less time writhing and more time moving.

Calcium‑ATPase pumps are the unsung heroes that end every contraction; when they falter, a spasm persists. The pump uses ATP to shuttle Ca²⁺ back into the sarcoplasmic reticulum, restoring the low‑calcium resting state. Adequate magnesium acts as a co‑factor, ensuring the pump runs efficiently. Dehydration thins the extracellular fluid, which diminishes ion conductivity and slows the pump’s activity. Likewise, potassium deficits raise the resting membrane potential, making it harder for repolarization to occur promptly. Regular intake of leafy greens, nuts, and legumes supplies both magnesium and potassium in bio‑available forms. Hydration should be measured not only by volume but also by electrolyte content; water alone may dilute plasma sodium. Stretching after activity promotes circulation, delivering nutrients to fatigued fibers and removing metabolic waste that can impede pump function. In summary, supporting the calcium‑ATPase pump with proper nutrition, hydration, and post‑exercise recovery reduces the likelihood of prolonged cramps.
Yo, they dont tell u that big pharma pushes those magnesium pills so they can keep u buying more supplements. Look, if u drink enough coconut water or eat bananas, the body usually gets what it needs. The "research" about needing extra mags is often funded by the very companies selling the tablets. Stay skeptical and stick to whole foods.
Honestly, anyone who skips water and still expects to avoid cramps is just delusional. Your excuses about "I’m too busy" are pathetic, and the fact that you ignore basic electrolyte balance shows a sheer lack of common sense. Stop whining, start drinking, and maybe you’ll stop being the walking example of a clueless athlete. The science is crystal clear, yet you act like it’s optional.
Think of a muscle spasm as a tiny rebellion inside your body; the fibers refuse to obey the king’s order to relax. It’s a reminder that even our biology loves drama, turning a simple contraction into a philosophical lesson about control. Yet, unlike existential crises, a spasm can be soothed with a stretch, a sip of electrolyte‑rich fluid, and a few mindful breaths.
Hey everyone, just wanted to add a friendly reminder that muscle health is a community effort. No matter your background, staying hydrated, stretching regularly, and eating balanced meals benefits all of us. If you’re new to fitness, start with short, gentle stretches and gradually increase intensity. Remember, consistency beats intensity when building long‑term resilience.
When you look at the cascade of events that lead to a muscle cramp, you realise it isn’t just a random mishap but a series of physiological missteps that can be traced back to very specific deficiencies. First, the nerve impulse fires, releasing acetylcholine, which is perfectly normal; the problem begins when calcium floods the sarcoplasmic reticulum and stays there longer than it should. The calcium‑ATPase pumps, which normally clear the excess, become sluggish in the presence of low magnesium, creating a bottleneck. Dehydration exacerbates this by reducing the extracellular volume, making it harder for ions to move across membranes. A lack of potassium further raises the threshold for repolarization, meaning the muscle fiber stays in a depolarized state. Fatigued muscle fibers also accumulate lactic acid, which interferes with enzymatic activity necessary for calcium reuptake. The net effect is a sustained cross‑bridge cycle that locks the muscle in a painful contraction. If you ignore these signals and continue to push through the pain, you risk chronic tightness and even tendon strain. Nutrition plays a huge role; foods rich in magnesium such as pumpkin seeds, legumes, and dark leafy greens provide the necessary co‑factor for the ATPase pumps. Likewise, bananas, sweet potatoes, and avocados supply potassium, which stabilises membrane potentials. Hydration should include electrolytes-plain water won’t replace sodium, chloride, or trace minerals lost through sweat. In practice, a balanced diet coupled with mindful hydration can dramatically lower the frequency of spasms. For athletes, a post‑exercise recovery protocol that includes gentle stretching, foam rolling, and a drink with a balanced electrolyte profile is essential. Lastly, chronic or severe cramps may signal underlying conditions like hyperparathyroidism or nerve compression, so consulting a medical professional is advisable if simple measures fail. Understanding the exact chain of events gives you the power to intervene at multiple points, preventing that dreaded knot from forming in the first place.
Building on the earlier advice, it's important to recognize that different muscle groups may respond uniquely to various interventions. For example, calf muscles often benefit from calf‑raising stretches performed after a warm shower, whereas hamstrings may feel relief with yoga‑style forward folds. Tailoring the approach to the specific muscle can accelerate recovery and reduce recurrence.
Just because the internet says magnesium is a miracle cure doesn’t mean you need to pop pills every day; most people get enough from a balanced diet, and over‑supplementing can cause diarrhea and other issues.
People love to claim that “cramps only happen to old people,” yet you can see a runner double‑over after a sprint if they skip a proper warm‑up, so the myth is just that-a myth.
Sure, cramps are just nature’s way of saying “take a break.”
Alright folks, remember that a quick static stretch right after the spasm can reset the muscle spindle, and a warm compress will boost blood flow, helping the calcium‑ATPase pump do its job faster; keep it simple, stay consistent, and you’ll see fewer nighttime leg cramps.
Hydration tip: sip a glass of water with a pinch of sea salt after a bout of exercise – it feels refreshing and helps replenish electrolytes! 😊
Whoa! Imagine your muscle as a tiny orchestra that suddenly gets stuck on a single, painful note – that’s a spasm, and it’s downright dramatic!
It’s absolutely shocking how many people ignore basic nutrition and then blame “mysterious” cramps for their laziness; honestly, it’s a moral failing to neglect such simple health basics.
Keep your chin up! Small daily habits like a quick stretch and a glass of water will make a big difference over time.
These foreign diet trends that push exotic super‑foods are just a marketing ploy; stick to good old British vegetables and proper hydration, not some imported hype.
Ugh, another post about “miracle cures” – I could write a drama about people chasing that hype all day, but honestly, it’s just exhausting.
For anyone looking for a step‑by‑step plan: 1) Drink 500 ml of electrolyte‑rich fluid before activity. 2) Perform dynamic stretches targeting the muscles you’ll use. 3) After exercising, do static holds for 30 seconds per muscle group. 4) Finish with a gentle massage or foam roll. 5) Keep a hydration log for a week to identify patterns. Follow this routine and you’ll drastically cut down on cramp frequency.
Wow!!! This is exactly what the community needed – let’s flood the thread with tips, emojis, and high‑energy encouragement! 📣💪 Stay hydrated, stretch often, and keep those muscles happy!!!
Great discussion, everyone. Remember, consistency in hydration, balanced electrolytes, and regular stretching are the simplest ways to keep cramps at bay.