People assume generic drugs are just cheaper copies of brand-name meds. And for the most part, they’re right. But when a patient switches from one generic to another-or even back to the brand-and suddenly feels off, things get confusing. Is it the drug? The dose? Or something else entirely?
Why Do People Think Generics Interact Differently?
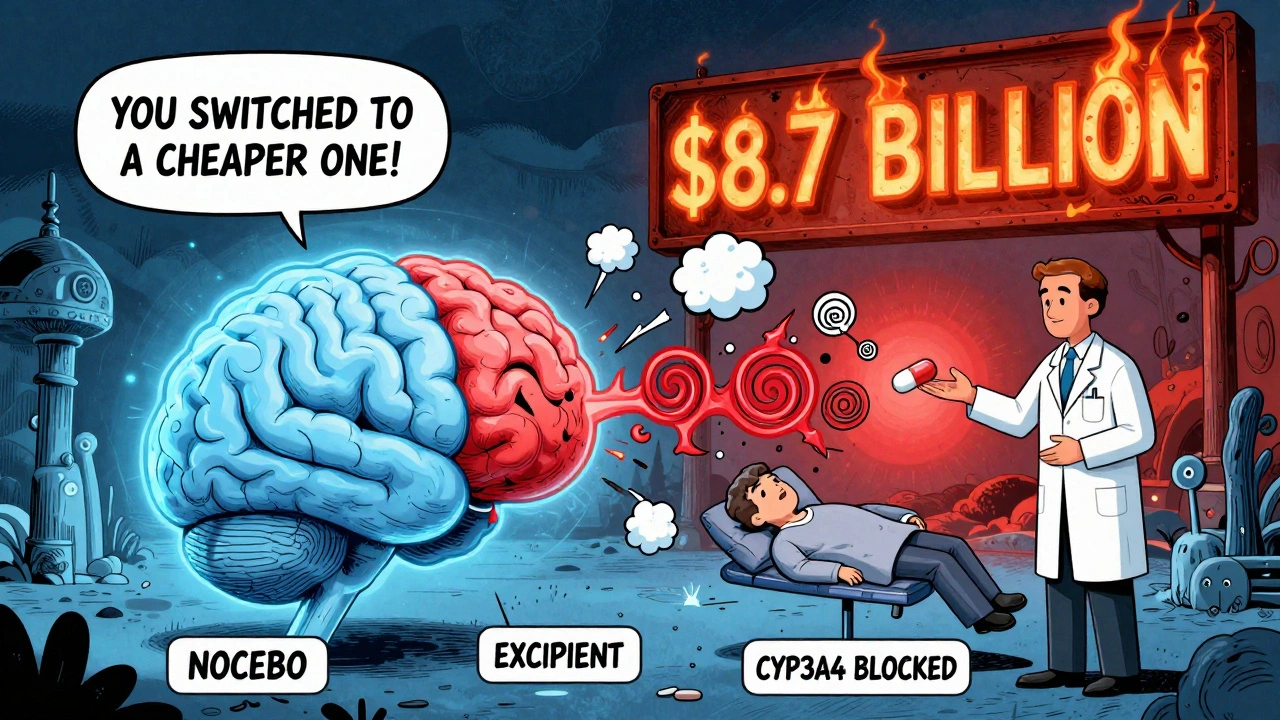
It’s not magic. It’s not conspiracy. It’s mostly noise. A 2022 Kaiser Family Foundation survey found nearly half of patients believe generics work differently than brand-name drugs. Over a quarter said they felt more side effects with generics. But when researchers dug into medical records, only 3.7% of those reports matched actual physiological changes. The rest? Psychological, misattributed, or misdiagnosed. The truth is, the active ingredient in a generic drug must be identical to the brand-name version. That’s not a suggestion-it’s a legal requirement enforced by the FDA. If the active ingredient doesn’t match, the drug doesn’t get approved. So if you’re taking a generic version of simvastatin, you’re getting the exact same molecule as the brand. That means the same interactions: grapefruit juice still blocks its breakdown. Fluconazole still spikes blood levels by 300-400%. The mechanism doesn’t change just because the pill is white instead of blue. So why the complaints? One big reason: inactive ingredients. These are the fillers, dyes, binders, and preservatives that hold the pill together. They don’t treat your condition. But they can irritate you. A 2021 case in the Journal of the American Pharmacists Association described a patient who developed severe stomach upset after switching from brand-name levothyroxine to a generic version. The brand used lactose-free fillers. The generic? Lactose. The patient had a mild intolerance they didn’t know about. The drug worked fine. The filler didn’t.When the Difference Actually Matters
Not all drugs are created equal in how tightly their levels need to be controlled. For most medications-antibiotics, blood pressure pills, antidepressants-a 10-20% variation in how much of the drug enters your bloodstream doesn’t matter. Your body adjusts. But for drugs with a narrow therapeutic index, even small changes can be dangerous. These include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (seizure control)
- Digoxin (heart rhythm)
What Really Causes Interaction Problems?
The real culprits behind bad reactions aren’t the generics. They’re:- Drug-drug interactions: Like taking fluoxetine with tramadol. Both raise serotonin. Together, they can trigger serotonin syndrome.
- Drug-food interactions: Grapefruit juice is the classic. It blocks an enzyme (CYP3A4) that breaks down over 85 drugs-including some statins, blood pressure meds, and immunosuppressants. This happens whether the drug is generic or brand.
- Drug-condition interactions: Diphenhydramine (Benadryl) can worsen glaucoma by increasing eye pressure. It doesn’t matter if it’s the generic or brand. The active ingredient is the same.

The Nocebo Effect: When Expectations Hurt
This is one of the most misunderstood parts of the issue. The nocebo effect is the opposite of the placebo effect. Instead of feeling better because you believe a treatment works, you feel worse because you believe it won’t-or will harm you. A 2021 study in JAMA Internal Medicine found patients told they were switching to a “cheaper generic” reported more side effects-even when they were still taking the exact same pill. Their brains expected trouble. Their bodies responded. Dr. Michael Cohen of the Institute for Safe Medication Practices put it plainly: “If a generic appears to interact differently, it’s almost always due to factors like inconsistent dosing, patient psychology, or undiagnosed conditions.” In a review of 42 cases where patients claimed new reactions after switching to generics, 38 were traced to miscommunication, dosing errors, or unrelated health changes. Only four involved real pharmacological differences-and two of those were due to excipients, not the active drug.What You Should Do
If you’re on a medication with a narrow therapeutic index:- Stick with the same generic manufacturer if possible. Ask your pharmacist if they can fill your prescription with the same brand of generic each time.
- Don’t assume a switch is harmless. Even if it’s “the same drug,” your body may need time to adjust to new fillers.
- Keep a log. Note when you switch generics and what symptoms appear. Was it the same day? A week later? Did your diet change? Did you start a new supplement?
- Ask your pharmacist: “What’s in this version that’s different from the last one?” They can tell you about excipients like lactose, gluten, or dyes.
- Don’t blame the generic without evidence. If you feel off, check for new medications, foods, or illnesses first.
Why This Matters
The cost difference between brand and generic can be huge. A 30-day supply of brand-name levothyroxine might cost $80. The generic? $4. That’s not a minor savings-it’s life-changing for people on fixed incomes. But if fear of interactions keeps people from using generics, the system pays the price. A 2023 Health Affairs analysis found that misplaced concerns over generics lead to 1.2 million unnecessary brand-name prescriptions every year in the U.S.-costing the healthcare system $8.7 billion. That money could fund cancer screenings, mental health services, or insulin for people who can’t afford it.The Bottom Line
Generics don’t interact differently because they’re generic. They interact the same way because they contain the same active ingredient. The few exceptions-like lactose in thyroid meds or sodium benzoate in sertraline-are rare, documented, and avoidable with better communication. The real issue isn’t the science. It’s the story we tell ourselves. That generics are inferior. That cheaper means worse. That switching pills is risky. It’s not. Not for most people. Not for most drugs. The system works. The data backs it. The science is clear. Trust the active ingredient. Watch the labels. Talk to your pharmacist. And don’t let fear cost you more than it should.Are generic drugs less safe than brand-name drugs?
No. Generic drugs are required by the FDA to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. The only differences are in inactive ingredients, which rarely cause problems. The FDA approves over 9,700 generic drugs each year, and their safety profile matches that of brand-name drugs.
Can switching between generic brands cause side effects?
It’s possible, but uncommon. For most medications, switching between generic manufacturers won’t change how you feel. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-even small changes in inactive ingredients can affect absorption in sensitive people. If you notice new symptoms after switching, talk to your pharmacist. They can check if the fillers changed and help you stick with one manufacturer if needed.
Do generic drugs have the same drug interaction warnings as brand-name drugs?
Yes. The FDA requires generic drug labels to include the same interaction warnings as the brand-name version. In a 2022 audit, 100% of generic labels met this requirement. If your brand-name pill says to avoid grapefruit juice or alcohol, so does the generic. The active ingredient determines the interaction-not the brand name.
Why do some people feel worse on generics?
Often, it’s not the drug-it’s the mind. The nocebo effect means people feel worse because they expect to. Studies show patients told they switched to a cheaper generic report more side effects-even when the pill hasn’t changed. Other times, it’s due to new inactive ingredients (like lactose or dyes) or unrelated changes like diet, stress, or new medications. Only about 13% of reported differences are linked to actual pharmacological changes.
Should I avoid generics if I’m on warfarin or thyroid medication?
No, but be smart. Generics for these drugs are safe and effective. However, because small changes in blood levels can be risky, it’s best to stick with the same generic manufacturer once you find one that works. Don’t switch brands unless necessary. Monitor your INR or TSH levels closely after any switch. Talk to your pharmacist about the filler ingredients-they can help you avoid ones you’re sensitive to.

bro i switched to generic lisinopril and my head started throbbing like a drum machine 😩 thought i was dying. turned out i was just stressed and the pill looked different. now i just stare at it for 10 seconds before swallowing like it’s a magic trick.
I’ve been on levothyroxine for 12 years and switched generics four times. The first time, I felt foggy for a week-didn’t know why. Then I noticed the new bottle had ‘lactose’ in the ingredients. I didn’t even know I was mildly intolerant. My doc didn’t mention it. My pharmacist didn’t mention it. No one did. I just thought I was getting worse. It’s not the drug. It’s the invisible stuff. The stuff they don’t advertise. The stuff you only learn about after you’ve spent three months Googling ‘why do I feel like garbage after pills?’
The FDA?!! The FDA is a corporate puppet! They approve generics with 80-125% variability?!! That’s not science-that’s corporate greed disguised as regulation! And don’t get me started on the dye in the pills-FD&C Yellow No. 5 is linked to ADHD, anxiety, and heart palpitations! They’re poisoning us under the guise of ‘cost savings’! I’ve seen the documents-there’s a secret clause in the 2019 amendment that lets them skip bioequivalence testing for ‘low-risk’ drugs! I’m not paranoid-I’m informed!
generic = cheaper. same pill. stop overthinking.
I just want to say how much I appreciate this post-it’s so easy to feel alone when you’re the one who ‘feels weird’ after a switch, especially when everyone else says ‘it’s all in your head.’ But you’re right: it’s not always in your head. Sometimes it’s the filler. Sometimes it’s the stress of change. Sometimes it’s both. I’m a nurse, and I’ve seen patients cry because they think they’re ‘broken’ after switching to a generic. I always sit with them. I ask about sleep, diet, new meds. I check the pill’s ingredients. And I remind them: your body isn’t failing you. The system just didn’t prepare you for the tiny details. You’re not crazy. You’re just paying attention. And that’s a good thing.
everyone says generics are fine but when you’re on warfarin and your INR jumps from 2.4 to 4.1 after switching from one generic to another? that’s not ‘nocebo’. that’s a near-stroke. and no one in the system takes it seriously. they just say ‘oh, maybe you ate more spinach.’
It is, without a doubt, a matter of empirical evidence, statistical significance, and regulatory fidelity. The notion that psychological factors dominate the perception of pharmacological efficacy is not only substantiated by peer-reviewed literature but also corroborated by longitudinal cohort analyses conducted by the National Institutes of Health. To assert otherwise is to undermine the very foundation of evidence-based medicine.
my aunt took generic metformin and got a rash. she swears it was the pill. doctor said it was stress. she died last year. i still think it was the generic. they don’t tell you what’s in em.
Oh, darling, the nocebo effect is the most deliciously tragic irony of modern pharmacology-a symphony of anxiety conducted by Big Pharma’s silent orchestra. We’ve been conditioned to equate price with potency, like a Victorian lady mistaking a knockoff porcelain teacup for a Meissen masterpiece. The pill is the same. The panic? Exquisitely bespoke. And yet-we cling to the ritual of the blue tablet, as if color were a sacrament. How profoundly human.
It’s not about the active ingredient-it’s about the epistemology of trust. We don’t just ingest molecules; we ingest narratives. The generic is a blank canvas upon which we project our anxieties about capitalism, healthcare inequality, and the erosion of bodily autonomy. The lactose? Merely a semiotic trigger. The real interaction is between the self and the system. And frankly? It’s not the pill that’s unstable. It’s the myth of the ‘identical’ drug. We’ve been sold a lie wrapped in a white capsule.